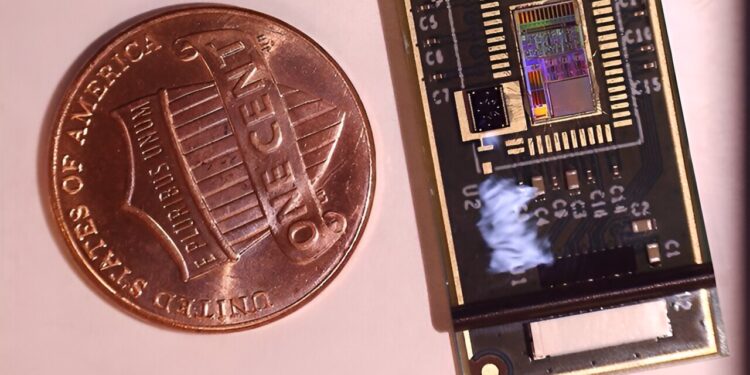
The microchip sensor is slightly larger than a coin. Credit: StethX and Georgia Institute of Technology.
Wheezing, a high-pitched whistling sound, is a common indicator of chronic respiratory diseases, including asthma and chronic obstructive pulmonary disease (COPD), due to inflammation and swelling of the airways.
As of 2023, nearly 9% of all adults in the United States had asthma, and COPD remains a leading cause of death in the United States.
Early detection and management of asthma and COPD are critical. Globally, asthma and COPD are underdiagnosed (20–70% for asthma and up to 81% for COPD). Additionally, the U.S. Centers for Disease Control and Prevention estimates that asthma is uncontrolled in 50% of children and 62% of adults, leading to frequent, severe episodes that can lead to increased emergency room visits and missed days from school and work.
Although digital stethoscopes are an improvement over traditional stethoscopes, they pick up airborne noise, which interferes with wheeze detection.
There is a need for an advanced technological solution that could be used as a screening tool in the clinic and for remote monitoring of patients, which would allow doctors to intervene early.
Researchers at the Georgia Institute of Technology have developed a deep learning (DL) model that they have paired with a wearable patch equipped with a highly sensitive sensor that can automatically detect wheezing. The deep learning model has the potential to classify respiratory diseases, which could speed up their diagnosis and treatment. The results of the pilot study on patients were published in Biosensors.
What Doctors Are Doing Now
Doctors typically use digital stethoscopes (the gold standard) to listen for and record abnormal lung sounds such as wheezes and crackles, which are clicking, popping noises that can accompany wheezing. They listen to each recording to determine whether it is wheezing, crackling, or normal breath sounds.
The standard method for classifying data as whistles is to perform a computerized time-frequency analysis that uses a checklist (i.e., an algorithm) to determine whether a whistle meets certain requirements. However, the algorithm is not exhaustive, resulting in some cases not being considered, the researchers said.
A new portable patch
To address these problems, the researchers designed a new wearable device. The patch features a chip sensor that, unlike traditional microphones in digital stethoscopes, can detect tiny vibrations with high sensitivity and minimal distortion.
“Our sensitive patch has many advantages over traditional wheeze detection, which struggles to detect all variations of wheezes and crackles, which can lead to misdiagnosis,” said Farrokh Ayazi, Ph.D., lead author of the study and professor of electrical and computer engineering at the Georgia Institute of Technology.
“By incorporating the data from these whistling variations into a deep learning model and taking advantage of the sensor’s ability to eliminate ambient sounds, our detection method led to greater accuracy, sensitivity (it correctly identified the presence of a whistling sound) and specificity (it correctly identified the absence of a whistling sound) compared to the standard time-frequency approach,” he said.
Developing a deep learning model
Lung sound recordings were made from 52 patients in an outpatient asthma clinic or hospital. Twenty-five of the 52 patients were obese, which can compromise the quality of traditional lung recordings.
To obtain the recordings, patients wore the miniature patch on nine different sites on their chest. Data was recorded at each location while the patient took deep breaths for 30 seconds at a time. For comparison, doctors also obtained lung recordings using digital stethoscopes at the same chest sites.
Doctors listened to recordings from both sources and indicated whether they heard wheezing or not in a blinded experiment, then provided a diagnosis after clinical assessment. The labeled wheezes were very close between the digital stethoscope and the wearable patch, even in obese patients. The clinician-labeled data was fed into the deep learning model so that it could distinguish wheezing from normal breath sounds.
Comparison of the DL model to standard methods
The researchers compared the deep learning model to the standard time-frequency method for wheeze detection when paired with the patch or digital stethoscope.
The deep learning model combined with the patch consistently achieved the highest average accuracy, sensitivity, and specificity rates for wheeze detection: 95%, 96%, and 93%, respectively. This combination outperformed the time-frequency method combined with the patch or the digital stethoscope, and the deep learning method combined with the digital stethoscope.
The study has some limitations: the only automated component is the deep learning model, which limits its application to clinical settings, and the results need to be further validated in a larger and more diverse patient sample.
Looking to the future
The researchers envision two potential uses for the wearable patch. One is for short-term screening in the clinic and the other for long-term home monitoring. The researchers are developing a wireless version of the patch for remote monitoring that could transmit data to the patient’s doctor to facilitate treatment.
“This noninvasive, rapid analysis of a patient’s respiratory and pulmonary status could improve early detection of respiratory problems, particularly in obese patients who are at higher risk for asthma and COPD,” said Tiffani Lash, Ph.D., program director of the NIBIB’s Division of Health Information Technology (Informatics).
“Technology solutions like this have the potential to improve health outcomes and ease the burden on people living with these chronic diseases,” she said.
More information:
Brian Sang et al., An accelerometer-based wearable patch for robust respiration rate and wheeze detection using deep learning, Biosensors (2024). DOI: 10.3390/bios14030118
Provided by the National Institutes of Health
Quote:Wearable lung patch uses deep learning to detect asthma and COPD (2024, September 11) retrieved September 11, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.