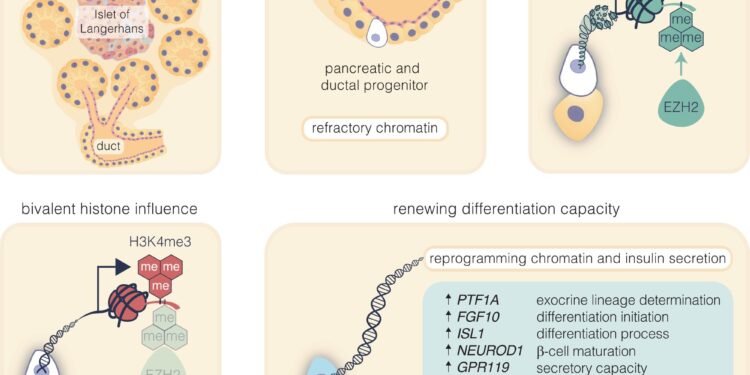
Pharmacological inhibition of EZH2 catalyzes pancreatic progenitor activation and β-cell maturation. The diagram depicts the progression from pancreatic multipotent progenitors to mature insulin-secreting β cells, highlighting the regulatory target of the EZH2 inhibitors GSK126 and Tazemetostat. Credit: Signal transduction and targeted therapy (2024). DOI: 10.1038/s41392-023-01707-x
Researchers are focused on the ultimate quest to regenerate insulin in pancreatic stem cells and replace the need for regular insulin injections.
Researchers from the Baker Heart and Diabetes Institute demonstrated in an article published in Signal transduction and targeted therapy that newly made insulin cells can respond to glucose and produce insulin after stimulation with two drugs approved by the U.S. Food and Drug Administration in as little as 48 hours.
Furthermore, they confirmed that this pathway for awakening insulin-producing cells is viable in age groups from 7 to 61 years, providing much-needed insight into the mechanisms underlying beta cell regeneration.
Using pancreatic cells from child and adult donors with type 1 diabetes and a non-diabetic person, a team led by Professor Sam El-Osta demonstrated how insulin-producing cells are destroyed in people with type 1 diabetes. type 1 can be regenerated into functionally glucose-sensing and secreting insulin cells.
In this latest study from the Human Epigenetics team, they show that small molecule inhibitors currently used to treat rare cancers and approved by the US FDA can quickly restore insulin production in pancreatic cells destroyed by diabetes.
Although current pharmaceutical options for treating diabetes help control blood sugar levels, they do not prevent, stop, or reverse the destruction of insulin-secreting cells.
The new therapeutic approach has the potential to become the first disease-modifying treatment for type 1 diabetes by facilitating the production of glucose-sensitive insulin by harnessing the patient’s remaining pancreatic cells, thereby allowing people living with diabetes to be potentially independent of 24-hour insulin injections.
This disease-modifying treatment also represents a promising solution for the significant number of Australians living with insulin-dependent diabetes, who represent 30% of type 2 diabetics.
The development of new pharmacological therapies aimed at restoring the function of the pancreas responds to the harsh reality of the shortage of organs among donors.
“We see this regenerative approach as an important step forward towards clinical development,” said Professor El-Osta. “So far, the regeneration process has been accidental and lacks confirmation. More importantly, the epigenetic mechanisms that govern such regeneration in humans remain poorly understood,” he said.
This research shows that 48 hours of stimulation with small molecule inhibitors is enough to restore insulin production from damaged pancreatic cells.
Dr. Keith Al-Hasani, principal investigator at JDRF, said the next step was to study the new regenerative approach in a preclinical model. The goal is to develop these inhibitors as drugs to restore insulin production in people with diabetes.
As work progresses, so does the need to translate quickly. More than 530 million adults are living with diabetes, and this number is expected to reach 643 million by 2030.
More information:
Keith Al-Hasani et al, EZH2 inhibitors promote β-type cell regeneration in young and adult type 1 diabetic donors, Signal transduction and targeted therapy (2024). DOI: 10.1038/s41392-023-01707-x
Provided by the Baker Heart & Diabetes Institute
Quote: Getting Closer to the Ultimate Quest to Regenerate Insulin in Pancreatic Stem Cells (January 2, 2024) retrieved January 2, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.