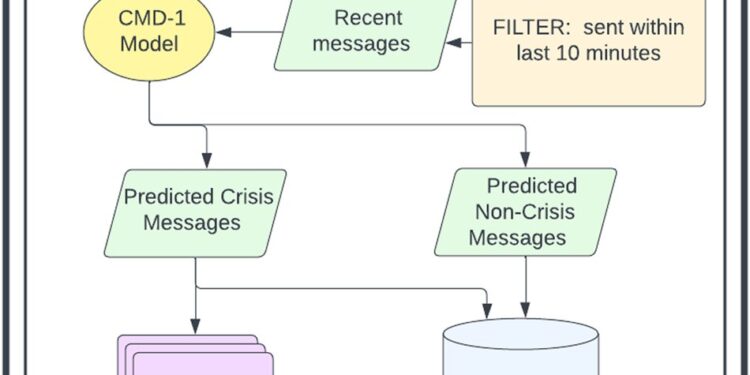
Diagram illustrating the flow of patient messages through the CMD-1 system during model deployment. Credit: npj Digital Medicine (2023). DOI: 10.1038/s41746-023-00951-3. npj Digital Medicine (2023). DOI: 10.1038/s41746-023-00951-3
Mental health needs are increasing. Today, one in five Americans lives with a mental health issue, and suicide rates over the past two decades have increased by more than 30 percent. Organizations like the National Alliance on Mental Illness (NAMI), which provides free support to people in crisis, have seen a 60% increase in the number of people seeking help between 2019 and 2021.
To cope with this increase, healthcare organizations and providers are turning to digital tools. Technology platforms such as crisis hotlines, text lines, and chat lines have trained and added staff to support patients in crisis. Despite this, dropped call rates for these organizations remain high at up to 25%. Additionally, the vast majority of these services are isolated from the callers’ clinicians.
One of the main factors contributing to this high dropout rate is that patient demand far exceeds the number of available responders. In 2020, the National Suicide Prevention Lifeline reported a response rate of just 30% for chat and 56% for text, leaving many patients in crisis without support. Additionally, these systems use a standard queuing method for incoming messages, where patients are served on a first-come, first-served basis, as opposed to their level of urgency.
What if these platforms could instead distinguish between urgent and non-urgent messages, thereby improving the efficiency of crisis triage?
That’s precisely what Stanford medical students Akshay Swaminathan and Ivan Lopez set out to do with their team of interdisciplinary collaborators, including clinicians and operational leaders from Cerebral, a national online mental health company, where Swaminathan leads data science.
The research team includes Jonathan Chen, Stanford HAI affiliate and assistant professor of medicine at the Stanford Center for Biomedical Informatics Research, and Olivier Gevaert, associate professor of medicine and biomedical data science at Stanford. The authors published their work in npj Digital Medicine.
Using natural language processing, the team developed a machine learning (ML) system called Crisis Message Detector 1 (CMD-1) that can automatically identify and sort messages, reducing processing times. Patient wait time from 10 hours to less than 10 minutes.
“For suicidal customers, the wait time was simply too long. The implication of our research is that data science and ML can be successfully integrated into clinician workflows, leading to dramatic improvements in at-risk patient identification and automation. these really manual tasks,” says Swaminathan.
Their results highlight the importance of applying CMD-1 to scenarios where speed is crucial. Lopez says: “CMD-1 improves the efficiency of crisis response teams, allowing them to handle a greater number of cases more effectively. With faster triage, resources can be allocated more efficiently, prioritizing urgent cases.
Empowering crisis specialists
The data the team used as the basis for CMD-1 came from Cerebral, which receives thousands of patient messages per day in its chat system. Messages can include topics as varied as scheduling appointments and refilling medications, as well as messages from patients in the event of an emerging crisis.
Starting with a random sample of 200,000 messages, they labeled patients’ messages as “crisis” or “non-crisis” using a filter that included factors such as crisis keywords and user IDs. patients who have already reported a seizure in the last week. Crisis messages that merit special attention include expressions of suicidal or homicidal ideation, domestic violence, or non-suicidal self-harm (self-harm).
“For mixed messages, like ‘I need help,’ we made a mistake calling it a crisis. From that sentence alone, you don’t know if the patient needs help making an appointment “you or to get out of bed.”, said Swaminathan.
The team also ensured that its approach complements, but does not replace, human review. CMD-1 surfaces crisis messages and sends them to a human for review as part of its typical crisis response workflow in a Slack interface. Any true crisis messages that the model fails to surface (false negatives) are reviewed by humans as part of the routine chat support workflow.
As Lopez says: “This approach is crucial to ensure that we reduce the risk of false negatives as much as possible. Ultimately, the human element in reviewing and interpreting messages ensures a balance between technological efficiency and compassionate care, which is essential in the context of mental health emergencies.
Given the sensitivity of the topic, the team was extremely conservative in how messages were categorized. They considered false negatives (missing a true crisis message) and false positives (incorrectly making a non-crisis message appear) and, in collaboration with clinical stakeholders, determined that the cost of missing a false negative was 20 times more undesirable than dealing with a false negative. Positive.
“This is a really key point when it comes to deploying ML models. Any ML model that performs classification (calling it ‘crisis’ or ‘no crisis’) must first generate a probability from zero to one. It generates a probability that the message is a crisis, but we have to choose this threshold, above which the model says crisis and below which the model says it is not a crisis. Choosing this threshold is a crucial decision, and this decision should not be made by the people building the model, it should be made by the end users of the model. For us, it’s the clinical teams,” says Swaminathan.
Remarkably, CMD-1 was able to detect high-risk messages with impressive accuracy (97% sensitivity and 97% specificity), and the team reduced response time for help seekers from over 10 hours to only 10 minutes. This timeliness is critical because rapid intervention has the potential to divert high-risk patients from suicide attempts.
The potential of ML in healthcare
Given their remarkable results, the team hopes that more machine learning models will be deployed in healthcare settings, which is currently rare because model deployment requires careful translation to clinical settings and attention particular to technical and operational considerations, as well as technological infrastructures.
“Often, data scientists create highly accurate ML models without fully addressing stakeholder concerns. As a result, these models, while technically competent, may create additional work or not integrate seamlessly into existing clinical workflows. “Scientists must involve healthcare professionals from the start, ensuring that models address the challenges they are designed to solve, streamline rather than complicate tasks, and fit organically into existing clinical infrastructure,” Lopez explains.
The CMD-1 development team took a unique approach of bringing together a cross-functional team of clinicians and data scientists to ensure the model meets key clinical thresholds and can generate meaningful results in a clinical operations environment real. “The compelling system developed here demonstrates not only an analytical outcome, but also the much more difficult work of integrating it into a real workflow that allows human patients and clinicians to join at a critical moment,” Chen explains.
This cross-functional approach, combined with the remarkable results of CMD-1, showed Swaminathan and Lopez how technology could be used to increase clinician impact. “This is where AI in medicine is heading, where we use data to make healthcare delivery more human, to make life easier for clinicians and empower them to provide higher quality care “, explains Swaminathan.
More information:
Akshay Swaminathan et al, Natural Language Processing System for Rapid Detection and Intervention of Chat Messages in Mental Health Crisis, npj Digital Medicine (2023). DOI: 10.1038/s41746-023-00951-3
Provided by Stanford University
Quote: Using natural language processing to detect mental health crises (January 17, 2024) retrieved January 17, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.