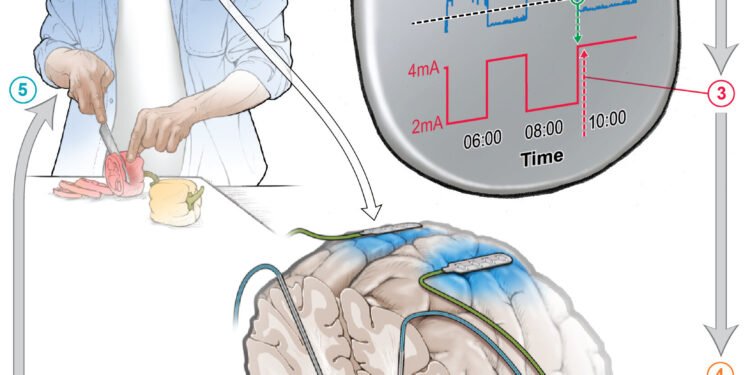
The implanted device responds to changes in brain signals, adjusting the amount of stimulation throughout the day, allowing individuals to go about their daily activities. Credit: Phillp Starr Lab
Two new studies from the University of California, San Francisco, are paving the way for personalized, 24-hour care for people with Parkinson’s disease using an implanted device that can treat movement problems during the day and insomnia at night.
The approach, called adaptive deep brain stimulation, or aDBS, uses AI-derived methods to monitor a patient’s brain activity for changes in symptoms.
When it detects them, it intervenes with precisely calibrated electrical impulses. The therapy complements the medications that Parkinson’s patients take to manage their symptoms, giving less stimulation when the medication is active, to prevent excessive movement, and more stimulation when the medication wears off, to prevent stiffness.
This is the first time that so-called “closed-loop” brain implant technology has been shown to be effective in helping Parkinson’s patients go about their daily activities. The device captures brain signals to create a continuous feedback mechanism that can reduce symptoms as they arise. Users can exit adaptive mode or stop treatment entirely using a handheld device.
For the first study, researchers conducted a clinical trial in four people to test the effectiveness of the approach during the day, comparing it to an earlier brain implant DBS technology known as constant or cDBS.
To ensure the treatment provided maximum relief for each participant, the researchers asked them to identify their most bothersome symptom. The new technology reduced these symptoms by 50 percent. The results are published Aug. 19 in Natural medicine.
“This is the future of deep brain stimulation for Parkinson’s disease,” said Philip Starr, MD, PhD, the Dolores Cakebread Professor of Neurological Surgery, co-director of the UCSF Movement Disorders and Neuromodulation Clinic and one of the study’s senior authors.
Starr has been laying the groundwork for this technology for more than a decade. In 2013, he developed a method to detect and then record abnormal brain rhythms associated with Parkinson’s disease. In 2021, his team identified specific patterns in these brain rhythms that correspond to motor symptoms.
“There has been a lot of interest in improving DBS therapy by making it adaptive and self-regulating, but it’s only recently that the right tools and methods have become available to allow people to use it long-term at home,” said Starr, who was recruited by UCSF in 1998 to start its DBS program.
Earlier this year, UCSF researchers led by Simon Little, MBBS, Ph.D., demonstrated Nature Communications that adaptive deep brain stimulation has the potential to alleviate the insomnia that afflicts many Parkinson’s disease patients.
“The big change we’ve made with adaptive deep brain stimulation is that we’re able to detect, in real time, where a patient is on the symptom spectrum and match them with the exact amount of stimulation they need,” said Little, an associate professor of neurology and senior author on both studies. Little and Starr are both members of UCSF’s Weill Institute for Neuroscience.
Restore the movement
Parkinson’s disease affects about 10 million people worldwide. It results from the loss of dopamine-producing neurons in the deep regions of the brain, responsible for controlling movement. The absence of these cells can also cause non-motor symptoms, affecting mood, motivation and sleep.
Treatment usually begins with levodopa, a drug that replaces the dopamine that these cells are no longer able to produce. However, excess dopamine in the brain when the drug is working can cause uncontrolled movements, called dyskinesias. When the drug wears off, the tremors and stiffness return.
Some patients then choose to have a standard deep brain stimulation device implanted, which provides a constant level of electrical stimulation. Constant deep brain stimulation can reduce the amount of medication needed and partially alleviate symptom fluctuations. But the device can also overcompensate or undercompensate, causing symptoms to swing from one extreme to the other throughout the day.
Closing the loop
To develop a DBS system that could adapt to changes in a person’s dopamine levels, Starr and Little needed to make the DBS capable of recognizing the brain signals that accompany different symptoms.
Previous research had identified patterns of brain activity linked to these symptoms in the subthalamic nucleus, or STN, the deep brain region that coordinates movement. This is the same area that deep brain stimulation stimulates, and Starr suspected that the stimulation would cut off the signals they were supposed to pick up.
So he found alternative signals in another region of the brain, called the motor cortex, that would not be weakened by DBS stimulation.
The next challenge was to determine how to develop a system that could use these dynamic signals to control DBS in an environment outside the laboratory.
Building on the results of adaptive DBS studies he had conducted at the University of Oxford a decade earlier, Little worked with Starr and his team to develop an approach to detect these highly variable signals across different levels of drugs and stimulation.
Over the course of several months, postdoctoral researchers Carina Oehrn, MD, PhD, Stephanie Cernera, PhD, and Lauren Hammer, MD, PhD, created a data analysis pipeline that could turn all of this into personalized algorithms to record, analyze, and respond to the unique brain activity associated with each patient’s symptomatic state.
John Ngai, Ph.D., who directs the Brain Research Through Advancing Innovative Neurotechnologies (The BRAIN Initiative) at the National Institutes of Health, said the study promises a marked improvement over current Parkinson’s treatment.
“This personalized, adaptive DBS embodies the core mission of the BRAIN Initiative, which is to revolutionize our understanding of the human brain,” he said.
A better night’s sleep
Continuous deep brain stimulation is intended to alleviate symptoms of daytime movement and does not typically relieve insomnia.
But over the past decade, there has been increasing recognition of the impact of insomnia, mood disturbances and memory problems on patients with Parkinson’s disease.
To fill this gap, Little conducted a separate trial that included four patients with Parkinson’s disease and one patient with dystonia, a related movement disorder.
In their article published in Nature CommunicationsFirst author Fahim Anjum, Ph.D., a postdoctoral researcher in the UCSF Department of Neurology, demonstrated that the device could recognize brain activity associated with various sleep states. He also showed that it could recognize other patterns that indicate a person is likely to wake up in the middle of the night.
Little and Starr’s research teams, including their graduate student Clay Smyth, have begun testing new algorithms to help people sleep. Their first study on sleep aDBS was published last year in Brain stimulation.
Scientists are currently developing similar closed-loop DBS treatments for a range of neurological disorders.
“We’re seeing this technology have a profound impact on patients, with potential not only for Parkinson’s disease, but also likely for psychiatric disorders like depression and obsessive-compulsive disorder,” Starr said. “We’re at the beginning of a new era of neurostimulation therapies.”
More information:
Carina Oehrn, Chronic adaptive deep brain stimulation versus conventional stimulation in Parkinson’s disease: a randomized, blinded feasibility trial, Natural medicine (2024). DOI: 10.1038/s41591-024-03196-z. www.nature.com/articles/s41591-024-03196-z
Fahim Anjum et al, Multi-night cortico-basal recordings reveal mechanisms of NREM slow wave suppression and spontaneous awakenings in Parkinson’s disease, Nature Communications (2024). DOI: 10.1038/s41467-024-46002-7
Provided by University of California, San Francisco
Quote:Taming Parkinson’s disease with self-adjusting brain pacemakers (2024, August 19) retrieved August 19, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.