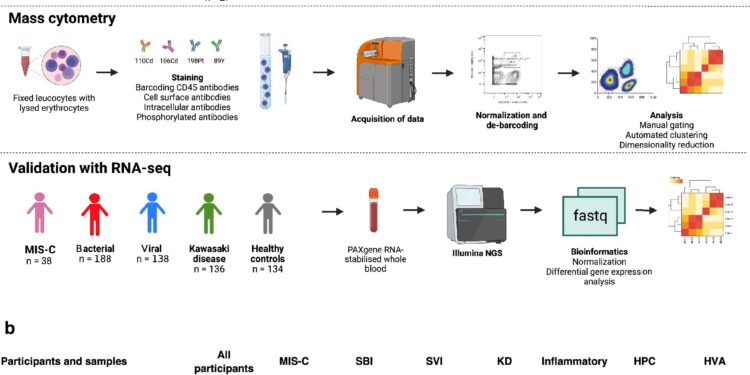
Schematic representation of the cohort studied, the experimental procedure and the samples analyzed. Credit: Nature Communications (2024). DOI: 10.1038/s41467-024-52246-0
A new study from King’s College London, Imperial College London and the University of Edinburgh has characterised the similarities and differences between immune cell profiles in children with different infections and inflammatory diseases.
The results, published in Nature Communicationscould help improve how we target immune system disruptions when treating these diseases.
Serious infections and inflammatory illnesses that cause fever (also called febrile illnesses) can be life-threatening for children. This is partly because they can prevent the immune system from working properly. This “immune dysfunction” makes the body less effective at eliminating infections and can overload the immune system, causing damage to the body.
Although their causes are different, severe febrile illnesses often have overlapping symptoms, and the immune dysfunction caused by these illnesses is also similar to that seen in sepsis. This can make diagnosis difficult. But understanding exactly what happens in the immune system in response to different febrile illnesses could help with diagnosis and highlight new ways to treat immune dysfunction in a more targeted manner.
In the study, the team looked at different groups of immune cells in blood samples taken from 128 children with different febrile illnesses, including multisystem inflammatory syndrome of childhood (MIS-C) associated with COVID-19 infection, severe bacterial infection, severe viral infection, and Kawasaki disease (a severe inflammatory disease in children), over the course of their illness.
“We found that severe bacterial infection and MIS-C overlap immunologically, although they are caused by very different factors,” said Dr Michael Carter, co-senior author of the study with Dr Harsita Patel of Imperial College London.
Using state-of-the-art mass cytometry equipment (which allows for the identification of individual cells), studies of cell function and immunoassays, the team found that two groups of white blood cells (neutrophils and T cells) were disrupted in children with MIS-C and severe bacterial infection, despite the different causes of the disease. They also found decreased levels of interferons – proteins that help clear viruses from the body – in children with severe viral infection.
The research was led by Professor Manu Shankar-Hari of the University of Edinburgh and Professor Michael Levin of Imperial College London.
The team was motivated to study immune dysfunction in febrile illness after noting that during the COVID-19 pandemic, the number of children being admitted to hospitals around the world with what looked like symptoms of a serious bacterial infection, including high fever, red eyes, conjunctivitis, rashes, and very low blood pressure, increased. In reality, the children were suffering from MIS-C, a condition that can develop about four weeks after COVID-19 infection.
“Currently, our treatments for immune dysfunction are poor and do not target individual children. In the future, by studying the immune system in much more detail, we hope to be able to develop therapies that can address the immune response in a much more targeted way and improve outcomes for our patients,” says Dr. Carter.
More information:
Harsita Patel et al, Shared neutrophil and T cell dysfunction is accompanied by a distinct interferon signature during severe febrile illness in children, Nature Communications (2024). DOI: 10.1038/s41467-024-52246-0
Provided by King’s College London
Quote:Study sheds new light on immune dysfunction in children with severe infections and inflammatory diseases (2024, September 23) retrieved September 23, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.