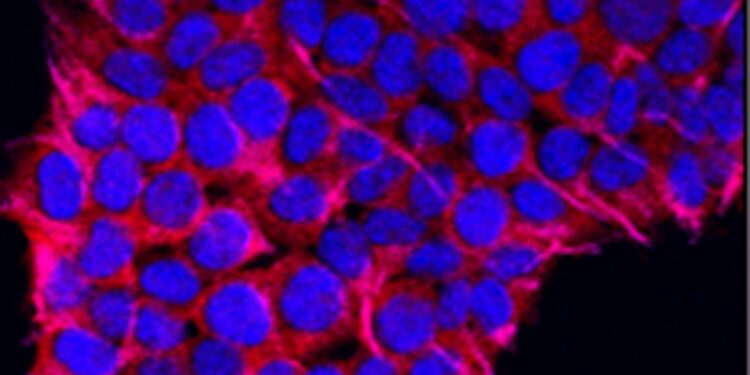
Credit: Unsplash/CC0 Public Domain
More than two decades ago, a research team in the lab of David Hafler, a researcher at Yale and Harvard at the time, discovered a type of T cell in humans that weakens the immune system. They later discovered that these so-called regulatory T cells, when defective, are an underlying cause of autoimmune diseases, particularly multiple sclerosis (MS). However, for many years, the mechanism behind this dysfunction remained unclear.
In a new Yale-led study, a team of researchers finds that this loss of immune regulation is triggered by an increase in PRDM1-S, a protein involved in immune function, triggering a dynamic interplay of multiple genetic and environmental factors, including high salt intake.
The results, published in the journal Scientific translational medicinealso reveal a new target for universal treatment of human autoimmune diseases.
The research was led by Tomokazu Sumida, assistant professor at Yale School of Medicine (YSM), and Hafler, the William S. and Lois Stiles Edgerly Professor of Neurology and professor of immunobiology at Yale.
“These experiments reveal a critical underlying mechanism for the loss of immune regulation in multiple sclerosis and likely other autoimmune diseases,” said Hafler, who is also chair of Yale’s Department of Neurology. “They also shed light on how regulatory T cell (Treg) dysfunction occurs in human autoimmune diseases.”
Autoimmune diseases, which are among the most common disorders in young adults, are known to be affected by genetic and environmental factors, including vitamin D and fatty acid deficiency. In a previous study, Sumida and Hafler found that high salt levels also contribute to the development of multiple sclerosis, an autoimmune disease of the central nervous system. Specifically, they observed that high salt levels induce inflammation in a type of immune cell called CD4 T cells, while causing a loss of function in regulatory T cells. They found that this is mediated by a salt-sensitive kinase, or enzyme essential for cell signaling, known as SGK-1.
For this new study, the researchers used RNA sequencing to compare gene expression in MS patients with healthy individuals. In MS patients, the researchers identified upregulation, or increased expression, of a gene called PRDM1-S (primate-specific transcription factor), also known as BLIMP-1, which is involved in regulating immune function.
The researchers found that PRDM1-S led to increased expression of the salt-sensitive enzyme SGK-1, which led to disruption of regulatory T cells. Additionally, they found similar overexpression of PRDM1-S in other autoimmune diseases, suggesting that it may be a common feature of regulatory T cell dysfunction.
“Based on these findings, we are now developing drugs that can target and reduce PRDM1-S expression in regulatory T cells,” Sumida said. “And we have initiated collaborations with other Yale researchers using novel computational methods to increase regulatory T cell function to develop new approaches that will work in human autoimmune diseases.”
The study was conducted with Bradley Bernstein and Manolis Kellis, longtime collaborators of Hafler’s at the Broad Institute of MIT and Harvard, and several other research institutions.
Other authors from the Yale lab include neurologist Matthew R. Lincoln and postgraduate research assistants Alice Yi, Helen Stillwell and Greta Leissa.
More information:
Tomokazu S. Sumida et al, An autoimmune transcriptional circuit drives FOXP3+ dysfunction of regulatory T lymphocytes, Scientific translational medicine (2024). DOI: 10.1126/scitranslmed.adp1720
Provided by Yale University
Quote:Study reveals molecular mechanism behind multiple sclerosis and other autoimmune diseases (2024, August 28) retrieved August 28, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.