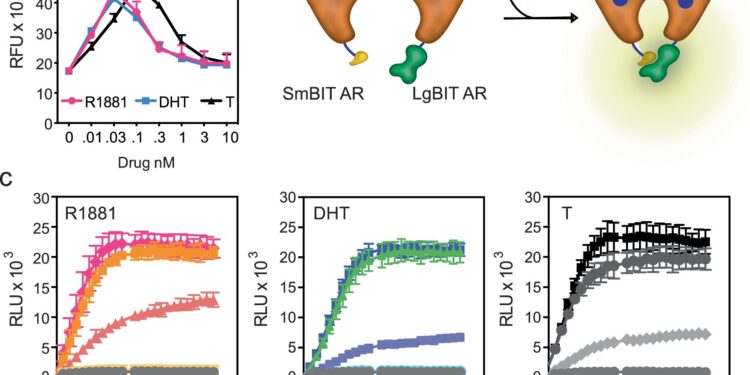
Low-dose androgens do not facilitate receptor dimerization. Credit: Nature Communications (2024). DOI: 10.1038/s41467-024-52032-y
A therapeutic paradox has recently emerged in prostate cancer: blocking testosterone production stops tumor growth early in the disease, while increasing the level of the hormone can delay disease progression in patients with advanced disease.
The inability to understand how different levels of the same hormone can lead to different effects on prostate tumors has been a barrier to the development of new therapies that exploit this biology.
A study conducted by the Duke Cancer Institute, carried out in the laboratory of Dr. Donald McDonnell and published in Nature Communicationsprovides the necessary answers to this riddle.
Researchers have discovered that prostate cancer cells have a system that allows them to proliferate when testosterone levels are very low. But when hormone levels are raised to resemble those found in a normal prostate, the cancer cells differentiate.
“For decades, the goal of endocrine therapy in prostate cancer has been to achieve absolute inhibition of the function of the androgen receptor, the protein that senses testosterone levels,” said lead investigator Rachid Safi, Ph.D., research assistant professor in the Department of Pharmacology and Cancer Biology, Duke University School of Medicine.
“This strategy has proven to be very effective, and has significantly improved overall survival,” he said. “Unfortunately, most patients with advanced metastatic disease who are treated with drugs that inhibit androgen signaling will progress to an aggressive form of the disease for which treatment options are limited.”
Prostate cancer cells respond differently to different doses of androgens. Credit: Nature Communications (2024). DOI: 10.1038/s41467-024-52032-y
Using a combination of genetic, biochemical and chemical approaches, the research team defined the mechanisms that allow prostate cancer cells to recognize and respond differently to different levels of testosterone, the most common androgen hormone.
It’s actually quite simple. When androgen levels are low, the androgen receptor is encouraged to “go it alone” in the cell. In doing so, it activates pathways that cause cancer cells to grow and spread. However, when androgens increase, the androgen receptors are forced to “pair up,” creating a form of the receptor that stops tumor growth.
“Nature has designed a system in which low doses of hormones stimulate cancer cell proliferation and high doses cause differentiation and suppress growth, allowing the same hormone to perform multiple functions,” McDonnell said.
In recent years, clinicians have begun treating patients with advanced, treatment-resistant prostate cancer using a monthly injection of high-dose testosterone in a technique called bipolar androgen therapy, or BAT. Failure to understand how this procedure works has hampered its widespread adoption as a standard treatment approach for prostate cancer patients.
“Our study describes how BAT and other similar approaches work and could help physicians select patients most likely to respond to this intervention,” McDonnell said. “We have already developed new drugs that exploit this novel mechanism and are bringing them to the clinic to be evaluated as treatments for prostate cancer.”
In addition to McDonnell and Safi, the study’s authors include Suzanne E. Wardell, Paige Watkinson, Xiaodi Qin, Marissa Lee, Sunghee Park, Taylor Krebs, Emma L. Dolan, Adam Blattler, Toshiya Tsuji, Surendra Nayak, Marwa Khater, Celia Fontanillo, Madeline A. Newlin, Megan L. Kirkland, Yingtian Xie, Henry Long, Emma Fink, Sean W. Fanning, Scott Runyon, Myles Brown, Shuichan Xu, Kouros Owzar and John D. Norris.
More information:
Rachid Safi et al, Androgen receptor monomers and dimers regulate opposing biological processes in prostate cancer cells, Nature Communications (2024). DOI: 10.1038/s41467-024-52032-y
Provided by Duke University Medical Center
Quote: Study resolves paradoxical effects of testosterone in prostate cancer (2024, September 4) retrieved September 4, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.