Credit: Unsplash/CC0 Public Domain
A Ludwig Cancer Research study has identified a metabolic switch in immune system T cells that is critical to the generation of memory T cells—which confer long-lasting immunity to previously encountered pathogens—and a T cell subtype present in tumors that triggers anti-tumor responses during immunotherapy.
Edited by Ping-Chih Ho and Alessio Bevilacqua of Ludwig Lausanne and published in the current issue of Sciences ImmunologyThe study identifies PPARβ/δ, a master regulator of gene expression, as this critical molecular switch. Ho, Bevilacqua, and colleagues also show that malfunction of the switch compromises T cell “memory” of previously encountered viruses and the induction of anticancer immune responses in mice.
“Our results suggest that we may be able to activate this switch pharmacologically to improve the effectiveness of cancer immunotherapies,” Ho said.
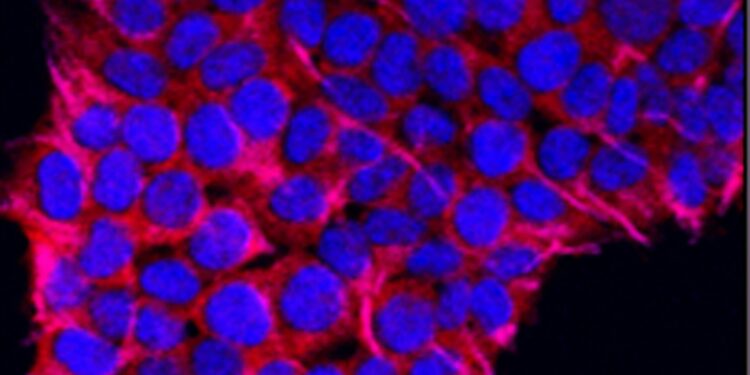
When the killer (or CD8+) T cells, which kill diseased and cancerous cells, are activated by their target antigen. They activate metabolic pathways that most other healthy cells use only when they are starved of oxygen. This type of metabolism, which involves a metabolic process known as aerobic glycolysis, supports multiple processes essential to the killer T cell’s ability to proliferate and destroy its target cells.
Most killer T cells die after clearing an infection. A few, however, transform into central memory CD8 cells+ T cells (Tcm) that persist in the bloodstream to establish what we call immunity: the ability to mount a rapid and lethal response to the same pathogen if it is encountered again. To achieve this transformation, T cells turn off aerobic glycolysis and adapt their metabolism to persist long-term in tissues or circulation. How exactly they do this was unknown until now.
Recognizing that PPARβ/δ activates many metabolic processes characteristic of Tcms, Ho, Bevilacqua, and colleagues hypothesized that it might play a key role in Tcm formation. They examined immunological gene expression data collected from yellow fever vaccinees long after vaccination and, as expected, found that PPARβ/δ was produced abundantly in their Tcms.
Their studies in mice revealed that PPARβ/δ is activated in T cells not during the peak phase of the immune response to viral infection, but when this response wanes. In addition, CD8+ T cells are unable to make the metabolic switch required to become circulating Tcms if they do not express PPARβ/δ. Disruption of its expression impairs the survival of these Tcms and of intestinal resident memory T cells after infection.
The researchers show that exposure of T cells to interleukin 15, an immune factor important for TCM formation, and their expression of a protein called TCF1 activate the PPARβ/δ pathway. It is already known that TCF1 is essential for the rapid expansion of TCMs when they encounter their target pathogen. The researchers show in this study that it is also important for the maintenance of TCMs.
It turns out that TCF1 expression is a characteristic of a subset of CD8+ T cells (progenitor exhausted T cells) found in tumors. These progenitor exhausted T cells follow one of two pathways: either they become completely lethargic, “terminally exhausted” T cells; or, with the appropriate stimulus, they proliferate to produce “effector” CD8 cells.+ T cells kill cancer cells. Checkpoint blockade immunotherapies, such as anti-PD-1 antibodies, can provide such a stimulus.
The observation that TCF1 modulates the PPARβ/δ pathway in T cells raised the possibility that it might also be essential for the formation and maintenance of progenitor-depleted T cells. The researchers showed that this was indeed the case. Deletion of the PPARβ/δ gene from T cells led to the loss of progenitor-depleted T cells in a mouse model of melanoma. They also demonstrated that the PPARβ/δ pathway limits the tendency of progenitor-depleted T cells to move toward terminal exhaustion.
To assess the therapeutic potential of their findings, Ho, Bevilacqua, and colleagues exposed T cells to a molecule that stimulates PPARβ/δ activity and used the treated cells against a mouse model of melanoma. These cells delayed the growth of melanoma tumors in mice more effectively than their untreated counterparts and exhibited the biochemical characteristics of progenitor-depleted T cells ready to generate cancer-killing progeny.
“Based on these results,” Bevilacqua said, “we suggest that targeting PPARβ/δ signaling could be a promising approach to enhance T cell-mediated antitumor immunity.
Exactly how this might be achieved in humans is a topic of further study that will no doubt be pursued by the Ho lab.
More information:
Alessio Bevilacqua et al, PPARβ/δ-orchestrated metabolic reprogramming supports the formation and maintenance of memory CD8+ T cells, Sciences Immunology (2024). DOI: 10.1126/sciimmunol.adn2717
Provided by the Ludwig Institute for Cancer Research
Quote:Study identifies metabolic switch critical to memory T cell generation and antitumor immunity (2024, August 24) retrieved August 24, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.