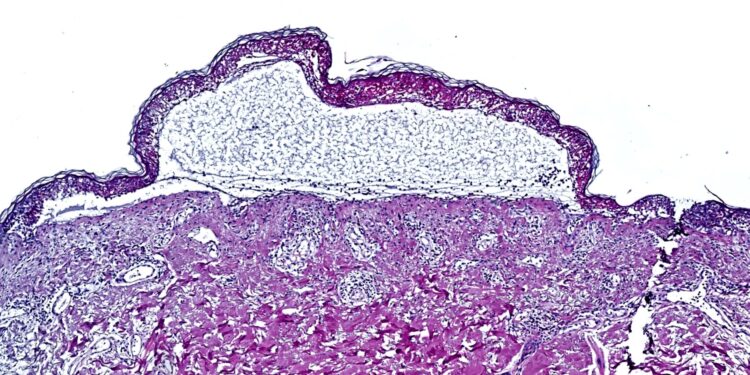
Epidermal detachment by toxic epidermal necrolysis. Credit: T. Nordmann
A global team of researchers from the Max Planck Institute for Biochemistry has made a discovery that helped save the lives of patients suffering from toxic epidermal necrolysis. This rare but often fatal reaction to common medications causes widespread skin peeling.
Using innovative spatial proteomics, one of the most advanced molecular biology tools, the team identified the JAK/STAT inflammatory pathway as the main driver of the disease. After validating their results in preclinical models, they successfully treated the first seven patients worldwide with JAK inhibitors, all of whom showed rapid and complete recovery.
Researchers used spatial proteomics to analyze skin samples from patients with toxic epidermal necrolysis. This cutting-edge approach, known as Deep Visual Proteomics, merges powerful microscopy with AI-based analysis, laser-guided microdissection, and ultimately ultra-high sensitivity mass spectrometry. They zoomed in on individual cells and studied them like never before, creating a map of the thousands of proteins driving this deadly reaction.
The work is published in the journal Nature.
Thierry Nordmann, first author, clinician-scientist at the Max Planck Institute for Biochemistry and senior dermatologist at the Ludwig Maximilians Universität München explains: “By applying spatial proteomics to archived patient samples suffering from toxic epidermal necrolysis, we were able to isolate and accurately analyze individual cell types and understand what is really happening in these patients’ skin.
“We identified a striking hyperactivation of the JAK/STAT inflammatory pathway, revealing an opportunity to intervene in this deadly disease with JAK inhibitors, a class of drugs already used to treat other inflammatory diseases, such as atopic dermatitis. or rheumatoid arthritis.”
Toxic epidermal necrolysis is a rare but extremely serious adverse reaction to common medications, such as allopurinol (used to treat gout) or certain antibiotics. It causes widespread blistering and peeling of the skin. With a mortality rate of up to 30 percent, it quickly transforms from a seemingly harmless rash into a potentially fatal illness. Until now, there was no effective therapy, with treatment limited mainly to supportive care.
The team validated their results through various preclinical studies, including in vitro models and two separate mouse models. The results have been consistent and extremely positive: JAK inhibitors show real potential in the treatment of this devastating disease. These findings were bolstered by a global collaboration across six countries, demonstrating the power of partnership to solve pressing medical challenges.
A new therapy for patients?
Partnering with clinical teams led by Chao Ji from the First Affiliated Hospital of Fujian Medical University in China, they administered JAK inhibitors to patients suffering from toxic epidermal necrolysis. Remarkably, all seven patients experienced rapid improvement and full recovery after treatment.
Lars French, co-corresponding author and chair of dermatology at LMU Munich, says: “The new evidence that inhibition of the JAK/STAT pathway has the potential to reduce the high mortality of this serious adverse skin drug reaction opens the path to clinical trials aimed at regulatory approval of JAK inhibitors to address one of the most serious unmet needs in medicine.
While larger clinical trials are needed to confirm the efficacy and safety of JAK inhibitors in toxic epidermal necrolysis, this study provides hope for patients facing this devastating disease. This also opens new opportunities for drug reuse and development. The Max Planck Society has filed patent applications in collaboration with the Ludwig Maximilian University for the use of JAK inhibitors in the treatment of toxic epidermal necrolysis and related conditions, creating potential for further development.
“Our results not only open new avenues to treat this reaction, but also highlight the potential of spatial proteomics to lead to medical breakthroughs,” explains Matthias Mann.
“To our knowledge, this is the first time that a spatial omics technology has had an immediate and tangible impact in the clinic, identifying a treatment that has already changed people’s lives for good. This approach could be applied to a wide range of diseases. , potentially accelerating drug discovery in multiple areas of medicine. »
More information:
Matthias Mann, Spatial proteomics identifies JAKi as treatment for deadly skin disease, Nature (2024). DOI: 10.1038/s41586-024-08061-0. www.nature.com/articles/s41586-024-08061-0
Provided by the Max Planck Society
Quote: Spatial proteomics approach leads to life-saving treatment for fatal skin reaction (October 16, 2024) retrieved October 16, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.