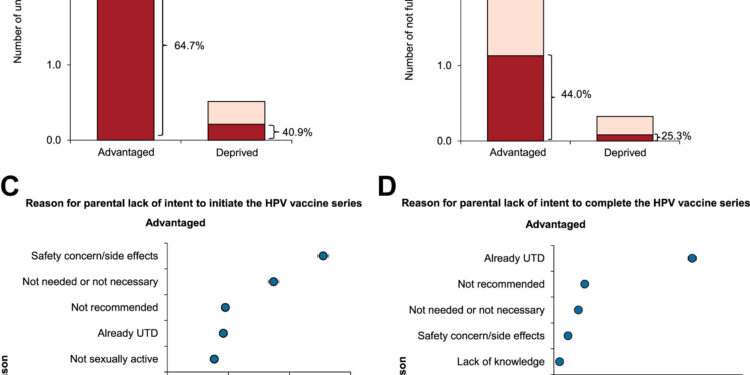
Lack of parental intention and reasons for lack of intention to initiate and complete HPV vaccine series in advantaged and disadvantaged group, NIS-Teen 2017-2021.A The figure illustrates the estimated population size of unvaccinated (PANEL A) and not fully vaccinated (PANEL B) adolescents and the proportion of parents not intending to start and complete the HPV vaccine series , respectively. The top five reasons for lack of parental intention to initiate (PANEL C) and complete (PANEL D) the HPV vaccine series in advantaged and disadvantaged groups are also listed. Abbreviations: HPV, human papilloma virus; NIS, National Immunization Survey; UTD, up to date AParental lack of intention to initiate the vaccine series was determined based on the response to the question “How likely is the adolescent to receive HPV vaccines in the next 12 months?” » The main reason for not intending to initiate the vaccine series was based on a response selected from a predefined list of reasons accompanying the question “What is the main reason why adolescents will not receive any HPV vaccine over the course of over the next 12 months? » AParental lack of intention to complete the vaccine series was determined based on the response to the question “How likely is the adolescent to receive all HPV injections in the next 12 months?” » The main reason for not intending to complete the vaccine series was based on a response selected from a predefined list of reasons accompanying the question “What is the main reason why adolescents will not receive all HPV vaccines over the next 12 months? » . Population estimates were derived from NIS-Teen survey weights. The proportion represents the adjusted and weighted survey design estimates derived using the full sample weights. Error bars represent 95% confidence intervals. Credit: The Lancet Regional Health – Americas (2024). DOI: 10.1016/j.lana.2024.100694
Parents of millions of adolescents do not intend to vaccinate their children against the human papillomavirus (HPV). Parents with higher socioeconomic status are less likely than parents with lower income or education to consider vaccinating their children.
HPV can cause six types of cancer in men and women, which is why public health advocates want more people to be vaccinated. The U.S. Healthy People 2030 program set a goal that 80% of adolescents receive the full series of vaccines, but that rate has stagnated at about 63% for adolescents.
Researchers at MUSC Hollings Cancer Center, aware of what is called the “inverse disparity,” in which people from low-income or minority communities have better HPV vaccination coverage than people from more advantaged communities, wanted to understand the level of vaccine hesitancy and discover the reasons that could lead to differences in vaccination coverage.
They used results from the National Immunization Survey-Teen, an annual telephone survey that covers several routine adolescent vaccines. Their findings are published this week in The Lancet Regional Health – Americas.
The researchers found that a majority of socioeconomically advantaged parents (65%) did not intend to vaccinate their adolescents, compared to 40% of parents in the disadvantaged group.
The reasons differed depending on the group. Advantaged parents generally cited safety concerns, while disadvantaged parents cited a lack of knowledge about the vaccine, lack of a recommendation from a primary care provider, or feeling that the vaccine is not necessary.
“Parents from socioeconomically advantaged households may reduce their child’s risk of HPV infection,” said lead author Kalyani Sonawane, Ph.D., a Hollings researcher and associate professor in the Department of Science. public health. “The side effects of the HPV vaccine may also be exaggerated in parents’ minds.”
Lead author Ashish Deshmukh, Ph.D., co-leader of the Cancer Control Research Program at Hollings, noted that white parents, whether advantaged or disadvantaged, showed a “widespread” lack of intention to be vaccinated.
Given that just over half of adolescents are white, their parents’ vaccination decisions have a significant impact on the herd immunity of the entire age group.
“This has population-level implications, because if most adolescents are white and from middle- or high-income families, and their parents perceive the vaccine to be unsafe, this impacts coverage. vaccine,” Sonawane said.
Previous studies indicated that minority parents were more likely to accept the vaccine and perceive the threat of HPV infection to be greater. They’re not necessarily wrong: Black and Hispanic women have higher rates of incidence and death from cervical cancer, which is almost always caused by HPV.
At the same time, Deshmukh has published studies over the past year showing that cervical cancer incidence rates are increasing among white women in low-income counties and among women in early childhood. thirty. Problems with access to preventative care and treatment could be behind higher mortality rates in all of these groups.
The HPV vaccine was first approved in 2006. It is recommended for adolescents, but can be given as a catch-up vaccine up to age 26. Because HPV is so widespread, the Centers for Disease Control and Prevention notes that almost everyone will be exposed at some point. a certain point – it is recommended to administer the vaccine well before there is a risk of exposure. However, after discussion with a doctor, it can be given to adults up to 45 years old.
There are hundreds of strains of HPV, most of which the human body eliminates on its own. Some of these strains, however, can progress to cancer of the cervix, head and neck, anus, penis, vagina, or vulva.
Sonawane said future studies could further subdivide the advantaged group based on income or education. This study included a middle group, in which parents had less than a high school diploma or earned less than 200 percent of the federal poverty level. In this mixed group, researchers found that higher education contributed more to HPV vaccination hesitancy than income.
More information:
Kalyani Sonawane et al, Factors associated with parental intentions to vaccinate against human papillomavirus among adolescents from socio-economically advantaged versus disadvantaged households: a national cross-sectional survey, The Lancet Regional Health – Americas (2024). DOI: 10.1016/j.lana.2024.100694
Provided by Medical University of South Carolina
Quote: Socioeconomically advantaged individuals are less likely to seek HPV vaccination for their children, researchers say (February 20, 2024) retrieved February 20, 2024 from
This document is subject to copyright. Apart from fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.