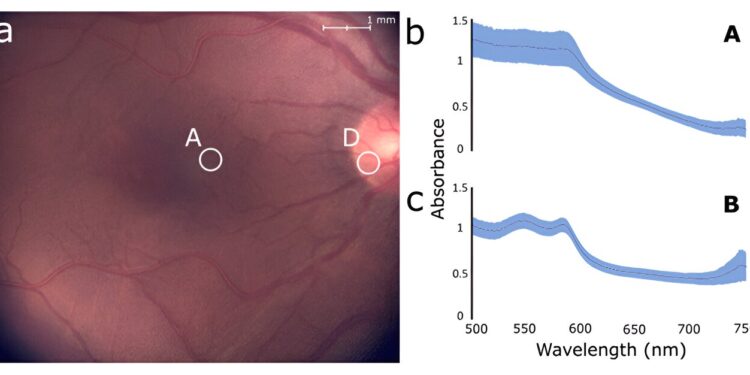
The proposed system can take detailed images of the fundus in real time while simultaneously measuring the spectral profile of a small target region, the position of which can be readjusted easily without requiring patient fixation. These capabilities facilitate the observation of spectral properties of specific structures or lesions in the retina, which can aid in the diagnosis of various conditions. Credit: Lapointe et al., doi 10.1117/1.JBO.28.12.126004.
Many eye diseases involve changes in the structure and function of different regions of the back of the eye, also known as the “fundus.” For example, fluorescent pigments and tiny yellowish deposits called drusen accumulate under the retina in age-related macular degeneration, and the degeneration of neurons called ganglion cells is a defining feature of glaucoma.
Interestingly, changes in the back of the eye are not limited to vision-related diseases alone. Certain neurological diseases like Parkinson’s disease and Alzheimer’s disease can cause changes in retinal nerves and blood flow.
Typically, eye care professionals rely on color imaging and CT scanning techniques to diagnose eye diseases. However, in recent decades, scientists have discovered that disease-related changes in the back of the eye also alter its spectral reflectance and emittance profiles. In other words, how light interacts with specific retinal structures at different frequencies can provide important diagnostic information to complement standard imaging methods.
As a result, tools and techniques for spectral analysis of light reflected or emitted from the back of the eye have gradually gained ground. Unfortunately, although many different methods have been proposed, they still suffer from significant limitations.
A common problem is that most spectroscopy-based methods can only make measurements over a broad region of the back of the eye, hampering their ability to detect fine spectral changes in small retinal structures. On the other hand, techniques for performing localized spectral measurements require patient fixation, which can be very tedious and uncomfortable.
To address these issues, a research team from Zilia Inc., Canada, led by Professor Dominic Sauvageau of the University of Alberta, developed a much more flexible system for targeted spectroscopy in the back of the eye. In their study, published in Journal of Biomedical Optics (JBO), they present the rationale for their design and demonstrate its potential through a series of extensive experiments.
The proposed system has a handful of key features that make it a more versatile and flexible alternative to existing systems. The entire device features a series of optical elements that essentially allow three different light paths to and from the back of the eye to coexist without obstructing each other. Specifically, lighting LEDs, a color camera, and a spectrometer can be used simultaneously to provide continuous color imaging and spectral measurements.
Additionally, the spectrometer section of the device focuses an LED onto a small region of the back of the eye, and the position of this region can be adjusted using simple mechanical actuators to rotate the beam splitter powering the camera and spectrometer.
“The user can select a target and move it to any location in the fundus region being imaged without any realignment or change in the fixation target while continuously receiving spectral information about the targeted sampled area,” explains Sauvageau.
This functionality makes it easy to perform spectral measurements from very specific anatomical structures, such as the optic nerve, retina, blood leak, fatty deposits or any type of lesion. Notably, the system can also be used to perform fluorescence measurements by adjusting the illumination source, which extends its applicability to detect an even wider variety of biomarkers.
The research team confirmed the capabilities and performance of their system through in vitro and in vivo experiments. The in vitro experiments involved targeting colored areas in a reference target with a grid-like pattern and taking spectral measurements of an eye model simulating a macula, blood vessels, a foreign body, and the optic nerve. In contrast, the in vivo measurements were performed on the retinas of eight healthy subjects, which showed differences in the spectral profiles of the optic nerve and the parafoveal region.
Taken together, the results of this study highlight the many advantages of the proposed design and could pave the way for better diagnostic protocols for eye diseases.
“Targeted ocular spectroscopy has the potential to assess the presence of different chromophores and fluorophores, such as hemoglobin, oxyhemoglobin, melanin and lipofuscin, associated with disease progression,” explains Sauvageau.
“This could open the door to changes in how we diagnose and treat eye diseases, and targeted ocular spectroscopy could become an increasingly important tool in eye care in the years to come.”
More information:
Nicolas Lapointe et al, Targeted spectroscopy in the fundus of the eye, Journal of Biomedical Optics (2023). DOI: 10.1117/1.JBO.28.12.126004
Quote: Scientists develop versatile imaging system that will help diagnose back-of-the-eye pathologies (December 18, 2023) retrieved December 18, 2023 from
This document is subject to copyright. Apart from fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.