Credit: Immunity (2024). DOI: 10.1016/j.immuni.2024.09.013
The ability to therapeutically manipulate the immune system presents a host of potential opportunities to treat infectious diseases, cancer, and other illnesses, but researchers must first fully understand the processes that shape immunity.
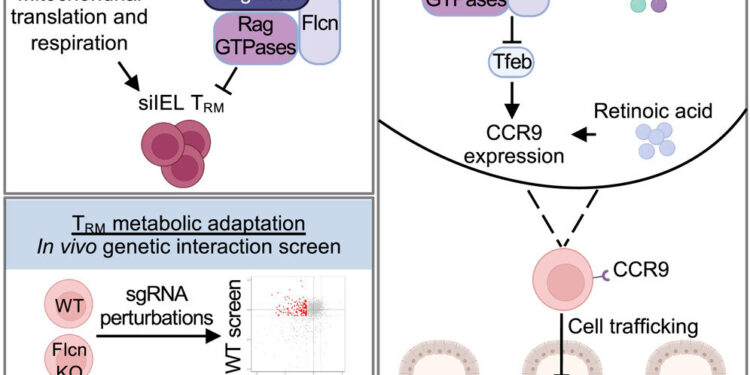
Scientists at St. Jude Children’s Research Hospital have added another piece to the puzzle, showing how metabolic factors influence tissue immunity in a complex interplay between nutrient availability, organelle biology and resident memory of tissues T (TRM) cell development.
The team discovered that TRM cells depend on mitochondrial activity for development and are inhibited by nutrient-sensing pathways in lysosomes. The results were published today in Immunity.
“We are excited to introduce a new layer of regulation in tissue immunity, which we believe will significantly improve our understanding of this area. Our results have the potential to inform new strategies for modulating tissue immunity, particularly to improve anti-infection responses. said corresponding author Hongbo Chi, Ph.D., St. Jude Department of Immunology.
The crucial role of memory T cells
CD8+ T cells play an essential role in defending against infections and cancer while promoting tissue health. During primary infections, they differentiate into effector cells, which provide immediate responses, and memory cells, which persist long-term for faster responses upon re-exposure.
TRM The cells are a specialized subset of memory cells that remain in tissues, providing rapid, localized responses by monitoring for signs of infection. Their ability to act as first responders enhances tissue-specific immunity, making them crucial for effective adaptive or long-term immunity.
“Our study focuses on tissue immunity, specifically examining TRM “These cells migrate to specific tissues, such as the lungs, intestines or skin, and establish long-term residence.
“They help provide the first line of defense against infections, and TRM-like cells are increasingly recognized for their role in the response to tumors.
TRM and TRM-like cells are of great interest due to their potential use in immunotherapy, as they provide rapid and localized immune responses to the site of infection or tumor growth. Their long-term presence in tissues guarantees lasting immunity and strong immune memory, allowing rapid reactions to previously encountered pathogens or cancer cells.
Organelle signaling and immune cell development
Researchers used CRISPR-Cas9 genetic screens to uncover critical signaling pathways influencing TRM cell development and differentiation. They found that TRM Cell formation depends on processes in cellular organelles called mitochondria. Additionally, signaling nodes at the lysosome (another organelle), such as Folliculin (Flcn), Ragulator and Rag GTPases, restrict TRM training and development.
“What we found particularly intriguing is that Flcn-mediated regulation is gut-specific, making it the first identified negative regulator of T.RM cells at a localized site,” Raynor said. “We are excited to target this pathway to improve the T in the long term.RM cells in the intestine, because our study shows that an increase in Flcn-deficient TRM cell levels provide better protection against infections.
Besides organelle signaling, the study also found that nutrient availability played a role in tissue immunity. Specifically, Flcn modulates the activity of transcription factor EB (Tfeb). Flcn–Tfeb signaling, induced by amino acid deprivation, contributes to TRM cell development.
The relationship links nutritional stress to cell fate decisions. Therefore, the Flcn–Tfeb axis is a regulatory pathway that coordinates immune responses to nutrient availability and lysosomal function.
“T cells migrate to various tissues and must adapt to the local nutrient environment. Our research uncovers the mechanisms by which T cells adapt to extracellular nutritional conditions and connect them to a key intracellular organelle, the lysosome,” Chi said.
“This finding further reinforces the emerging concept we have helped champion that nutrients serve as a unique type of signal, known as “Signal 4,” to enable T cell immunity.”
This work highlights the metabolism-associated mechanisms that lead to an immune memory response in a highly tissue-specific manner, thereby presenting promising future applications such as dietary interventions, vaccination strategies, and personalized medicine approaches.
“We are particularly excited about the potential of nutrient and diet availability, as it is something that individuals can actively manage and apply. Exploring how modulating nutrition can significantly influence the establishment of immune responses stronger,” added Raynor.
More information:
Jana L. Raynor et al, CRISPR screens unveil nutrient-dependent lysosomal and mitochondrial nodes impacting the formation of intestinal tissue-resident memory CD8+ T cells, Immunity (2024). DOI: 10.1016/j.immuni.2024.09.013
Provided by St. Jude Children’s Research Hospital
Quote: Researchers show how nutrients and organelle signaling shape tissue immunity (October 15, 2024) retrieved October 15, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.