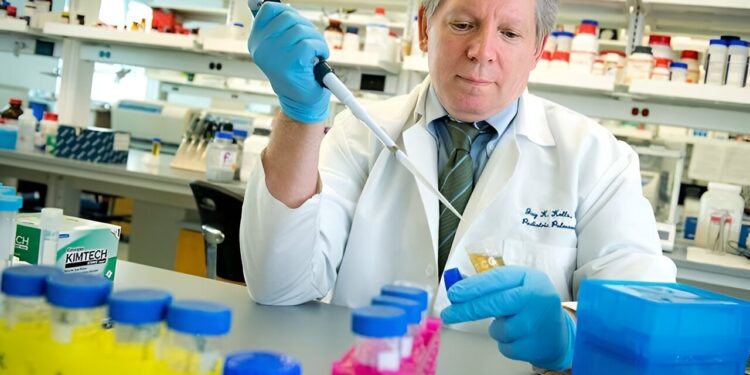
Tulane scientists have made crucial progress in developing a model to study a fungus that causes Pneumocystis pneumonia in immunocompromised patients and children. Credit: Paula Burch-Celentano
Scientists at Tulane University School of Medicine have developed a promising new model for studying a pneumonia-causing fungus that is notoriously difficult to grow in the laboratory.
Researchers were able to use precisely cut slices of lung tissue to study Pneumocystis species, a fungus that causes Pneumocystis pneumonia in immunocompromised patients and children.
This innovation overcomes a major obstacle in mushroom research – the difficulty of cultivating this pathogen outside of a living lung – so that scientists can more easily test new drugs to fight the infection. The fungus was recently listed as one of 19 priority fungal pathogens by the World Health Organization.
“Pneumocystis is probably the most common fungal pneumonia in children, and attempts to culture the organism have largely failed,” said corresponding author Dr. Jay Kolls, the John W Deming Professor of Internal Medicine. at Tulane. “So we haven’t had new antibiotics in over 20 years because they have to be tested in experimental animal studies.”
The Tulane model uses precision-cut lung slices that retain the complexity and architecture of lung tissue, providing an environment that closely mimics the conditions inside the lung. The results were published in mBio.
The researchers used mouse tissue to grow two forms of the Pneumocystis fungus, the trophy and the ascus, for up to 14 days. The viability tests and gene expression analysis they performed showed that the fungus survived over time in the model.
“This is the first time that the trophic and ascus forms of Pneumocystis have been maintained long-term outside of a mammalian host,” Kolls said.
The researchers confirmed the model’s potential for in vitro drug testing. When treated with commonly used drugs trimethoprim-sulfamethoxazole and echinocandins, Pneumocystis gene expression was reduced, indicating successful targeting of the fungus.
The Tulane technique reliably generates many uniform samples of lung tissue for experimentation from a single lung, enabling high-throughput testing.
“With optimization, we believe that precision lung slices could enable real growth of Pneumocystis and become a powerful tool for developing new drugs to treat this infection,” Kolls said. “This could significantly accelerate research into this pathogen.”
The study was led by Ferris T. Munyonho, a Tulane biomedical sciences graduate student and recipient of a Fulbright scholarship after earning his bachelor of science degree from the University of Zimbabwe.
More information:
Ferris T. Munyonho et al, Precision cut lung slices as an ex vivo model to study survival and antimicrobial susceptibility of Pneumocystis murina, mBio (2023). DOI: 10.1128/mbio.01464-23
mBio
Provided by Tulane University
Quote: Researchers make breakthrough in fight against major cause of fungal pneumonia (December 28, 2023) retrieved December 28, 2023 from
This document is subject to copyright. Apart from fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.