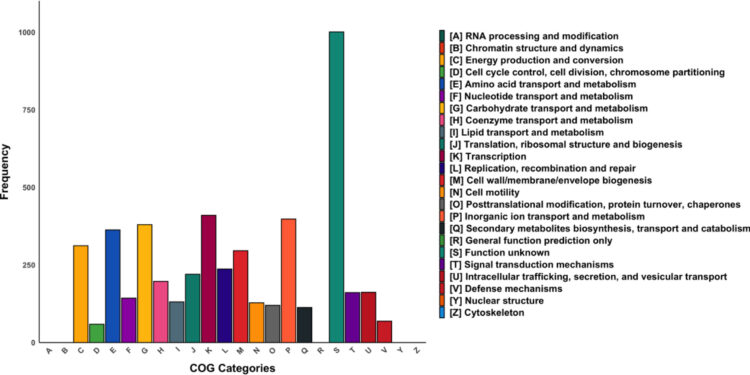
Quantitative KEGG analysis of genes identified in the UCI isolate. The bar graph illustrates the distribution of genes in the different KEGG categories found in the UCI isolate. Each bar represents a specific category of the KEGG pathway analysis, and the height of the bar corresponds to the number of genes identified in that category. The X axis shows the different KEGG categories, while the Y axis represents the number of genes found in each category. Credit: Journal of Hospital Infections (2024). DOI: 10.1016/j.jhin.2023.12.010
Researchers at the University of Limerick in Ireland have discovered a new species of bacteria resistant to antibiotics.
The discovery was made by researchers from the UL School of Medicine, who identified a new antibiotic-resistant bacterial species capable of colonizing patients in hospital settings.
The new bacterial species was discovered in the wastewater treatment system at University Hospital Limerick, as well as from swabs taken from a patient admitted to one of the hospital’s wards.
This follows an extensive and unique study in which researchers, in partnership with University Hospital Limerick and Queen’s University Belfast, delved deep into hospital sewage to find a reservoir of bacteria resistant to antibiotics.
The new study, led by Professor Colum Dunne, Director of the University of Limerick School of Medicine, and recently published in the Journal of Hospital Infectionsdetails the large-scale genomic and microbiological analysis carried out on the UHL wastewater treatment system, the results of which were correlated with samples taken from patients as part of the hospital’s cautious approach in microbiology and infection risk management.
Researchers detected, characterized and identified a new species of bacteria present in the hospital sewage system and which was also isolated from a patient colonized by the bacteria after his admission to hospital wards for treatment.
Laboratory analysis revealed that the new species is resistant to many commonly used antibiotics, including some reserved for resistant bacteria. Fortunately, the patient was asymptomatic and did not require treatment with these medications.
Antimicrobial resistance (AMR) is a major challenge that is directly responsible for more than a million deaths each year worldwide. AMR makes infections more difficult to treat and increases the risks associated with other medical procedures and treatments.
One of the problems associated with AMR is nosocomial infection, which occurs when people admitted to hospital for treatment become infected by microbes circulating in hospital wards.
The Limerick group has worked for more than a decade to better understand what these microbes are, where they are found and what drugs they are resistant to, helping to build systems to prevent and control disease outbreaks. these infections.
The analysis, called metagenome analysis because it is the study of the structure and function of all the DNA sequences of these samples, allowed a comprehensive understanding of the bacterial communities in the wastewater of the ‘hospital. It made it possible to profile all the antimicrobial resistance genes carried by the bacteria present.
Professor Colum Dunne, lead author and leader of the study, Director of the School, Chair of the Foundation and Director of Research at the UL School of Medicine, said: “Our research strategy highlights the focuses on clarifying real-world problems and seeking solutions. In this situation, the bacteria were isolated from a patient who had been swabbed as part of a routine safety process put in place with the support of the hospital leadership team.
“Unusually, the bacteria could not be identified using diagnostic approaches routinely used in hospital laboratories. Using data from our large-scale study of the hospital wastewater system and sequencing the genome of the new isolate, we confirmed two things: that the bacteria is present in the hospital system and the patient was colonized by the bacteria after admission to hospital.
“The bacterial family, called Pseudocitrobacter, has only recently been classified, and we found that our isolate is a new addition to this family, having never been reported elsewhere and having never been isolated from a human sample .”
“While this is an exciting microbiological finding, it is important that we emphasize that the patient remained colonized only, asymptomatic and did not merit antimicrobial treatment for this species.”
Professor Colum Dunne continued: “It is very likely that the identification of new bacterial species will occur more frequently. Hospitals around the world are high-use environments for pharmaceuticals, such as antibiotics, and in this type of ecosystem, mutations frequently occur.
“In our studies of these microbes, we are seeing the emergence of new patterns of antimicrobial resistance, new genes, new plasmids (transmissible DNA elements) encoding resistance, and potential for further colonization of patients.”
“In our hospital group, these risks are recognized. Our work has been made possible by a forward-looking approach to infection prevention and by the facilitation of research by hospital management. Such support is an indicator of a A best-in-class healthcare system practices proactive, solution-oriented research that can make a difference. We recognize this and look forward to continued collaborations between our universities and hospitals.
Study co-author Dr Nuala O’Connell, UL consultant and adjunct associate professor in clinical microbiology, explained: “It is fortuitous to have access to wonderful academic research scientists at UL and Queen’s University Belfast who could carry out specialist molecular testing. to help identify the new microbe. This allowed us to understand the potential route of acquisition, which will impact infection prevention and control strategies.
Professor Dunne highlighted the importance of collaboration between scientists and clinicians. “This is an example of innovation having a real impact on society. University researchers bring expertise and access to sophisticated molecular equipment which, combined with the clinical knowledge of hospital doctors and monitoring scientists, can help ensure patient safety. “
“It is likely that the analysis we have performed will become more widely available, less expensive, and will enable the identification of infectious agents more quickly, perhaps even through bedside or point-of-care testing, as as technology improves.”
Professor Brendan Gilmore, co-author and Professor of Pharmaceutical Microbiology at QUB, said: “This All-Ireland collaboration supports the importance of interdisciplinary academic and clinical research in the surveillance, identification and control of threats potential emerging bacterial infections in healthcare. system.”
The importance of the study was summarized by James Powell, a surveillance scientist at University Hospital Limerick.
“Recent advances in molecular techniques have allowed us to explore the microbial epidemiology of our patients and the hospital environment in ways we could not have imagined just a short time ago. It was an honor and privilege to be part of the research group studying this new bacterial isolate.
Dr Stephen Kelly, co-author and senior lecturer in pharmaceutical microbiomics at the QUB School of Pharmacy, added: “Studying this microorganism and its genome was very interesting, not only because of the challenges initial linked to the discovery of his identity, but also because of its clinical relevance. This research once again highlights the benefits of high-level collaboration between academic and clinical partners.
More information:
Stephen A. Kelly et al, A novel characterized multidrug-resistant Pseudocitrobacter isolated from a colonized patient while admitted to a tertiary teaching hospital, Journal of Hospital Infections (2024). DOI: 10.1016/j.jhin.2023.12.010
Provided by University of Limerick
Quote: Researchers discover new species of bacteria resistant to antibiotics (January 16, 2024) retrieved January 16, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.