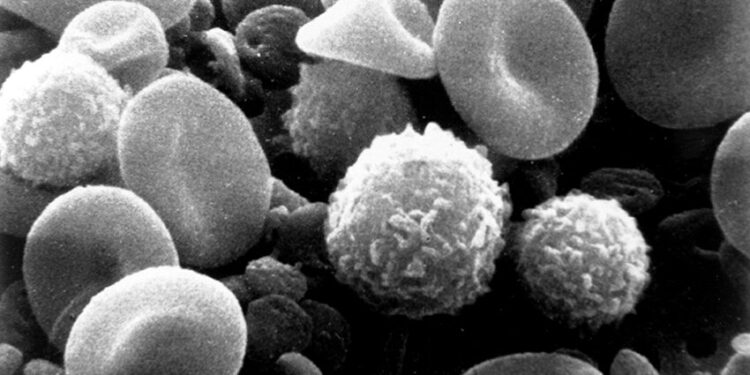
Myeloid immune cells alongside red blood cells in an electron micrograph of human blood. Credit: National Cancer Institute
Immunotherapies that mobilize the patient’s immune system to fight cancer have become a mainstay of treatment. These therapies, including CAR T cell therapy, have shown good results in cancers such as leukemias and lymphomas, but results have been less promising in solid tumors.
A team led by Penn State College of Medicine researchers has redesigned immune cells so that they can penetrate and kill solid tumors grown in the laboratory. They created a light-activated switch that controls protein function associated with cell structure and shape and incorporated it into natural killer cells, a type of immune cell that fights infections and tumors.
When these cells are exposed to blue light, they transform and can then migrate into tumor spheroids (3D tumors grown in the laboratory from mouse or human cell lines) and kill the tumor cells. This new approach could improve cellular immunotherapies, the researchers said.
The results are published this week in the Proceedings of the National Academy of Sciences. The researchers also filed a provisional application to patent the technology described in the paper.
“This technology is completely original. It is similar to CAR T cell therapy, but here the guiding principle is the ability of cells to infiltrate the tumor,” said lead author Nikolay Dokholyan, Professor G. Thomas Passananti at the Penn State College of Medicine and professor of biochemistry and molecular biology. “I don’t know of any other approach that comes close.”
CAR T cell therapy was first approved by the Food and Drug Administration in 2017 and has since demonstrated encouraging results for certain cancers, particularly blood cancers. T cells, a white blood cell of the immune system, are taken from a patient and engineered to produce a protein on their surface that binds to a specific target protein on cancer cells. When CAR-T cells are reinfused into the patient, they kill cancer cells with this target protein.
However, CAR-T cell therapy is less effective at treating solid tumors, which account for about 90% of adult human cancers and 40% of childhood cancers, Dokholyan said. Immune cells cannot infiltrate the dense network of proteins and other cells surrounding the tumor, and the hostile environment inhibits their tumor-fighting abilities.
Additionally, the enormous diversity of solid tumors makes it difficult to locate a specific target protein to attack. To improve cellular immunotherapies against solid tumors, Dokholyan said immune cells must be able to evade the solid tumor’s defenses.
Using computer modeling, the team designed and tested a light-controlled version of septin-7, an internal protein essential for maintaining a cell’s cytoskeleton, the structure that maintains shape and function. cellular organization. They inserted a light-sensitive domain into septin-7 to create what Dokholyan called “an allosteric regulator.”
The light-sensitive part of the protein is located far from the active site of the protein and does not interfere with the structure and function of the protein until it is triggered. The domain is activated by blue light, which turns protein function on and off.
They then redesigned human natural killer immune cells with the light-sensitive protein septin-7. In the presence of blue light, researchers observed that the normal functioning of septin-7 was disrupted. The cells also had a more elongated, spindle-shaped shape and larger protrusions extending outward, which helps the cell interact with its environment and move from one place to another.
“Even though natural killer cells are small, about 10 micrometers, upon activation of this protein by blue light, the immune cells change shape and can squeeze through tiny holes of about three micrometers. This is enough to infiltrate tumor spheroids and kill them from within,” Dokholyan said.
The researchers tested the engineered natural killer immune cells with two types of solid tumor spheroids, one created from human breast cancer cells and the other with human cervical cancer cells. In seven days, they killed the tumor cells.
In contrast, natural killer cells that had not been remodeled attacked the tumor spheroid from the outside but were unable to breach the tumor. Eventually, the tumor continued to grow. They also redesigned mouse immune cells and tested them with tumor spheroids made from mouse melanoma cells.
Although the results are strong, Dokholyan emphasized that this work is still in its preliminary stages and that additional research is needed to evaluate this technology for potential therapeutic use. He said he also hopes to explore other activation signals that may modulate protein function and cellular behavior.
Other authors of the Penn State paper include Todd Schell, professor of microbiology and immunology at Penn State College of Medicine; Brianna Hnath, doctoral student in biomedical engineering; Congzhou Mike Sha, joint MD/Ph.D. student Medical Scientist Training Program; and Lynne Beidler, research technologist. The first author, Jiaxing Chen, was a doctoral student at the time the research was conducted and is currently a postdoctoral researcher at the University of Pennsylvania.
More information:
Dokholyan, Nikolay V., Optogenetically engineered Septin-7 enhances immune cell infiltration of tumor spheroids, Proceedings of the National Academy of Sciences (2024). DOI: 10.1073/pnas.2405717121
Provided by Pennsylvania State University
Quote: Redesigned immune cells activated by blue light penetrate and kill solid tumors (October 21, 2024) retrieved October 21, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.