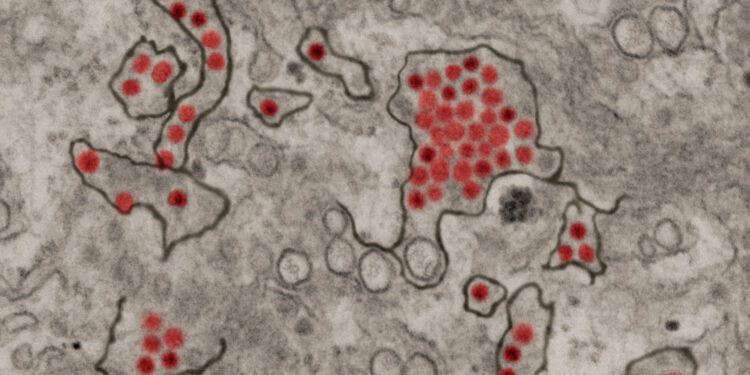
Zika virus particles (red) shown in African green monkey kidney cells. Credit: NIAID
A study by Brazilian researchers shows that people who contracted the Zika virus are at higher risk of developing severe dengue fever and being hospitalized. This discovery is very relevant for the development of a Zika vaccine.
According to the scientific literature, a second infection with one of the four known dengue serotypes is generally more serious than the first, but until now no correlation between this fact and the appearance of other diseases had been studied.
The study is published in the journal Tropical diseases neglected by PLOS.
The mechanism that exacerbates dengue infection following one case of Zika differs from that of two consecutive dengue virus infections, the authors conclude. Viral load is higher in the second episode of dengue, with elevated levels of inflammatory cytokines not seen in Zika.
The detection of other markers suggests that the increase in severity could be due to the activation of T cells, key parts of the immune system that help produce antibodies, in a pathogenic immune response called “original antigenic sin.”
The process involves what is called T cell memory, a response in which T cells produced during a previous infection stimulate the production of more T cells to fight a new infection. Because these new cells are not specific to the virus, they trigger an excessive release of inflammatory cytokines, which attack the body’s proteins and tissues, potentially leading to bleeding.
Researchers analyzed samples from 1,043 laboratory-confirmed dengue patients, identifying those who had previously been infected with Zika and dengue. The cases occurred in 2019 in São José do Rio Preto, a large city in the state of São Paulo, Brazil, considered hyperendemic for dengue since more than 70% of the population has been affected by the disease. Its climate and geography favor the circulation of arboviruses throughout the year. Dengue outbreaks occurred there in 2010, 2013, 2015, 2016 and 2019, with a record number of cases involving serotype 2.
“We concluded that prior dengue infection was not a risk factor for severity, probably because patients were already on their third or fourth infection. Prior Zika infection was, however, important and a factor. worsening during a second episode of dengue. This led us to suggest new mechanisms and renew our knowledge on the natural history of the disease”, declared to the FAPESP Agency Cássia Fernanda Estofolete, specialist in infectious diseases at the Faculty of Medicine of São José do Rio Preto (FAMERP) and first author of the article.
“Our results confirmed the results of a previous study of children with Zika in Nicaragua. Later, when they had dengue, the risk of severity increased. We showed the same thing (risk of severe dengue increased by previous Zika or dengue) for adults. “We also showed that ADE (antibody-dependent enhancement, in which – instead of providing protection – antibodies enhance virus entry into host cells and can exacerbate the disease) is not classic,” said corresponding author Maurício Lacerda Nogueira.
“This raises questions about what type of Zika vaccine to use and when is optimal: should it be given with a dengue vaccine to avoid this problem one after the other, for example? There are various possibilities , that it must be understood to ensure correct prescription. In Brazil it is even more important to give the dengue vaccine first due to the number of cases,” added Nogueira.
Case numbers
In November 2023, the number of dengue cases in Brazil exceeded the number reported in the 12 months of 2022, reaching 1,372,000, of which 1 million were confirmed between January and July (publication date of the last available bulletin). The states of São Paulo and Minas Gerais have recorded the highest number of cases, according to the Health Ministry.
Regarding Zika, the latest figures for 2023 are 4,773 probable cases, including 1,725 confirmed. Bahia and Rio Grande do Norte recorded the highest number of cases. Epidemiologists note that arbovirus diseases are generally underreported, because they are difficult to diagnose and because many people have mild symptoms and do not seek health services for treatment.
In 2016, when Zika outbreaks broke out in many parts of the world, Brazil accounted for more than 1.5 million of the 2.38 confirmed cases in the Americas. In 2019, South America experienced a dengue epidemic, with more than 3.13 million cases reported, four years after the appearance of Zika on the continent.
In March 2023, a dengue vaccine produced by a Japanese company gained approval from ANVISA, Brazil’s health monitoring agency, and this vaccine is now available in private clinics. The Butantan Institute is developing a fully indigenous dengue vaccine that will be distributed to public clinics. Development of a Zika vaccine is underway, but at an early stage.
Dengue and Zika are both flaviviruses, transmitted by the same mosquito (Aedes aegypti) and have similar symptoms, often making diagnosis difficult. Dengue is more serious because in addition to fever, headache, muscle and joint pain, rash and nausea, it can cause bleeding and even death.
Zika symptoms are milder, but the virus can cause serious problems in pregnant women and babies, such as microcephaly and possibly Guillain-Barré syndrome, a neurological disorder leading to paralysis.
Experts warn that Aedes mosquitoes and the diseases they transmit are appearing in temperate regions due to global warming and climate change. Deforestation also contributes to the increase in cases because mosquitoes have more predators in biodiversity hotspots.
Sample analysis
The study was carried out using samples from patients suspected of dengue fever, confirmed by RT-PCR. Samples were evaluated for history of dengue and Zika infection using an enzyme-linked immunosorbent assay (ELISA) developed by the FAMERP group in partnership with the laboratory of Lee Gehrke at the Massachusetts Institute of Technology (MIT) in the United States. The test was specifically developed to eliminate the high cross-reactivity between flaviviruses observed in commercial kits available on the market.
The analysis showed that patients with a history of Zika infection had a 2.34 times higher risk of developing severe dengue and a 3.39 times higher risk of hospitalization compared to controls (subjects without dengue and without a history of Zika). Relatively old age (over 59 years) was also a higher risk factor for severe forms of dengue and hospitalization.
With years of research behind them, Nogueira and his group published a 2021 study showing that previous dengue infection in pregnant women infected with the Zika virus does not increase the risk of giving birth to an affected baby of microcephaly.
Estofolete has now embarked on a new stage of research, extending the study period to cover dengue cases reported in 2022 and changing the serotype.
“The goal is not only to answer questions about severity, but also to find out whether the mechanism we detected is the same for all dengue serotypes, as this influences other factors and mechanisms. We “We don’t have a lot of accumulated knowledge about Zika vaccines,” he said.
More information:
Cassia F. Estofolete et al, Influence of previous Zika virus infection on the acute episode of dengue, Tropical diseases neglected by PLOS (2023). DOI: 10.1371/journal.pntd.0011710
Quote: Previous Zika infection increases risk of severe dengue fever and subsequent hospitalization, study concludes (February 6, 2024) retrieved February 6, 2024 from
This document is subject to copyright. Apart from fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.