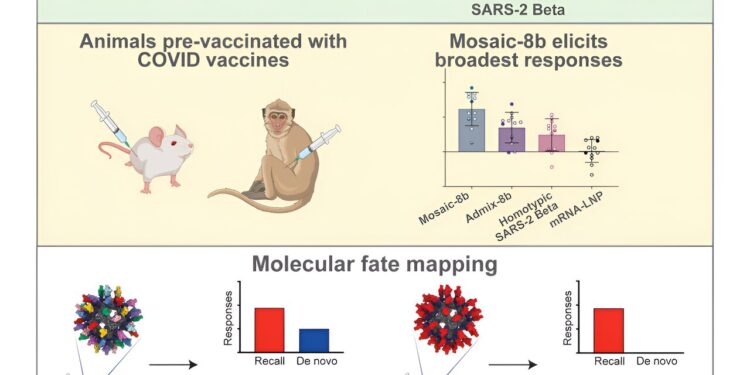
Graphic summary. Credit: Cell (2024). DOI: 10.1016/j.cell.2024.07.052
Researchers estimate that nearly all Americans have been exposed to SARS-CoV-2, the virus that causes COVID-19, either through infection or vaccination. This means we are no longer “immunologically naive”—that is, our immune systems are familiar with some variants of SARS-CoV-2. This familiarity may pose a challenge for vaccine development.
In immunology, the phenomenon of “original antigenic sin” or OAS is a colloquial term for the body’s first encounter with a virus, which can forever “bias” the immune response to produce antibodies tailored to the initial strain upon exposure, regardless of subsequent infections with other strains or boosters of vaccines designed for different viral variants.
Viruses like SARS-CoV-2, including the virus that caused the initial SARS outbreak in 2002, belong to a family called SARS-like betacoronaviruses, or sarbecoviruses. Sarbecoviruses have already caused two global health crises in the past 20 years, suggesting that a new sarbecovirus could cause a new epidemic or pandemic and highlighting the need for broad protection against viruses in this family. But does OAS pose a problem for future vaccines designed to broadly protect against sarbecoviruses and SARS-CoV-2 variants of concern?
This question is the subject of a new study in the Caltech lab of Pamela Björkman, the David Baltimore Professor of Biology and Biological Engineering and a Merkin Institute professor.
The study, titled “Mosaic Sarbecovirus Nanoparticles Elicit Cross-Responses in Pre-Vaccinated Animals,” is published in CellThe work was carried out in collaboration with researchers from Rockefeller University in New York and the University of Washington.
Researchers in the Björkman lab have developed and tested a new vaccine candidate called mosaic-8 that has shown potential to protect against several different types of sarbecoviruses, including SARS-CoV-2 and its variants.
In animal models, mosaic-8 induces the production of cross-reactive antibodies capable of neutralizing several sarbecoviruses and SARS-CoV-2 variants.
As the Mosaic-8 vaccine is being prepared for first-in-human clinical trials, scientists wanted to understand whether OAS would influence the composition of the antibodies induced—in other words, how would the Mosaic-8 vaccine influence antibody production in individuals who have already mounted immune responses to SARS-CoV-2, either through infection, immunization, or both? Would the Mosaic-8 vaccine elicit antibodies that are biased toward SARS-CoV-2, as OAS suggests, or would it still elicit broad and cross-reactive antibodies against multiple sarbecoviruses and variants?
The new study, described in a paper published in the journal Cell on August 27, looked at animal models that received COVID-19 vaccines and then mounted an immune response. In an encouraging step toward the development of the vaccine candidate, the team found that the Mosaic-8 gene elicits broadly protective cross-reactive antibodies in both previously exposed and immunologically naïve animals.
How Mosaic-8 works
When you get a vaccine against a certain pathogen, your body develops different antibodies to attack that pathogen and creates B cells that store a memory of how to create those antibodies. Like a lock and key, each antibody protein is specifically designed to attack a specific pathogen. There are billions of different B cells in your body, each encoding the ability to generate antibodies against specific viruses and other microbes.
After receiving a SARS-CoV-2 vaccine, the body produces many different antibodies that target different regions of the virus. Some of these regions, called conserved regions, are the same across variants. Antibodies that target conserved regions are more likely to protect against multiple different variants and similar viruses.
The Mosaic-8 vaccine is designed to elicit antibodies against conserved features of sarbecoviruses. The vaccine contains fragments from eight different sarbecoviruses. These fragments are regions of the virus’ spike protein called receptor-binding domains (RBDs). The spike protein and its RBDs are essential for the virus to infect a cell. The Mosaic-8 vaccine is therefore designed to induce the production of cross-reactive antibodies that target conserved regions of the RBDs and thus protect against multiple sarbecoviruses and SARS-CoV-2 variants of concern.
Mosaic-8 elicits broadly protective antibodies, regardless of prior exposure or vaccination
In the study, the team used mouse and non-human primate models to determine what types of antibodies were elicited by mosaic-8 after prior vaccination with three different COVID-19 vaccines.
The researchers first immunized the animals with mRNA vaccines similar to the Pfizer and Moderna vaccines or with AstraZeneca’s ChAdOx1 vaccine, vaccines widely available for humans, to replicate the situation in humans who are not immunologically naïve to SARS-CoV-2. After antibodies were induced by one vaccine, the animals were then immunized with the team’s Mosaic-8 vaccine containing RBDs from SARS-CoV-2 and seven related sarbecoviruses.
The researchers then looked at antibodies in the animals’ serum. They found that the Mosaic-8 vaccine boosted antibodies targeting conserved regions of the RBDs of both animal sarbecovirus variants and SARS-CoV-2, and also promoted the creation of new antibodies targeting regions specific to some of the seven RBDs of the animal sarbecovirus.
“Current COVID-19 vaccines are not specifically designed to generate a broad antibody response that might provide better protection against variants or related viruses,” says Alexander Cohen, a postdoctoral researcher and co-first author of the new study.
“We have developed a vaccine that provides broad protection against a wide spectrum of sarbecoviruses to prevent the next pandemic. Fortunately, our new results show that this vaccine works as expected to elicit broadly protective antibody responses in both previously exposed and immunologically naïve animals.”
After infection or vaccination, humans produce antibodies that target conserved regions of sarbecoviruses, but they are not the dominant type of antibodies produced by the body, said Jennifer Keeffe, lead researcher and co-first author of the study.
“The goal of our Mosaic-8 vaccine is to preferentially stimulate these types of antibodies so that the body makes more of them, thereby providing broader protection. We have observed the production of these cross-reactive antibodies in our previous studies in immunologically naïve animals, and we have now verified that generalized cross-reactive antibodies are also produced in pre-vaccinated animals. We look forward to confirming this result in our future clinical trials,” says Keeffe.
Phase 1 clinical trials to test the Mosaic-8 vaccine in humans are expected to begin in 2025.
More information:
Alexander A. Cohen et al, Mosaic sarbecovirus nanoparticles elicit cross-reactive responses in pre-vaccinated animals, Cell (2024). DOI: 10.1016/j.cell.2024.07.052
Cell
Provided by California Institute of Technology
Quote:Multi-purpose vaccine shows promise in presence of pre-existing immunity (2024, August 27) retrieved August 27, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.