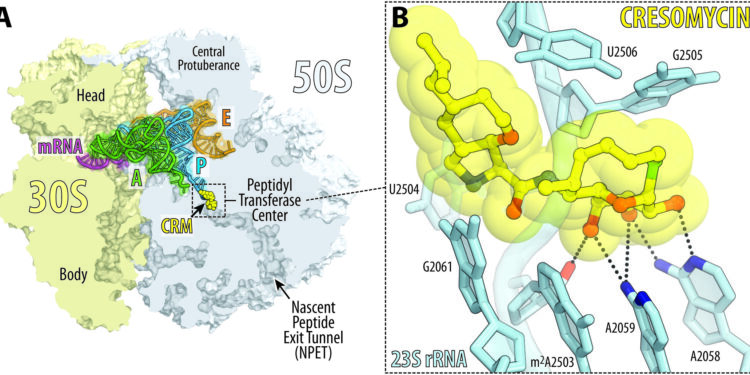
Overview and close-up of cresomycin bound to the bacterial ribosome of Thermus thermophilus. Credit: Yury Polikanov/University of Illinois at Chicago
A new antibiotic created by Harvard researchers overcomes antimicrobial resistance mechanisms that have rendered many modern drugs ineffective and are causing a global public health crisis.
A team led by Andrew Myers, Amory Houghton Professor of Chemistry and Chemical Biology, reports in Science that their synthetic compound, cresomycin, kills many strains of drug-resistant bacteria, including Staphylococcus aureus and Pseudomonas aeruginosa.
“While we do not yet know whether cresomycin and similar drugs are safe and effective in humans, our results show significantly improved inhibitory activity against a long list of pathogenic bacterial strains that kill more than a million people each year. year, compared to clinically approved antibiotics,” Myers said.
The new molecule demonstrates an improved ability to bind to bacterial ribosomes, which are biomolecular machines that control protein synthesis. Disruption of ribosomal function is a hallmark of many existing antibiotics, but some bacteria have evolved protective mechanisms that prevent older drugs from working.
Cresomycin is one of several promising compounds developed by Myers’ team, aiming to help win the war against superbugs. They will continue to advance these compounds through preclinical profiling studies.
The Harvard team’s new molecule is inspired by the chemical structures of lincosamides, a class of antibiotics that includes the commonly prescribed clindamycin. Like many antibiotics, clindamycin is manufactured by semisynthesis, in which complex products isolated from nature are modified directly for drug applications. Harvard’s new compound, however, is entirely synthetic and features chemical modifications inaccessible by existing means.
“The bacterial ribosome is nature’s favorite target for antibacterial agents, and these agents are the inspiration for our program,” said co-author Ben Tresco, a student at the Kenneth C. Griffin Graduate School of Arts and Sciences. “By leveraging the power of organic synthesis, we are limited almost solely by our imagination when designing new antibiotics.”
Bacteria can develop resistance to antibiotics targeting ribosomes by expressing genes that produce enzymes called ribosomal RNA methyltransferases. These enzymes remove components of the drug that are designed to latch onto and disrupt it, blocking the drug’s activity.
To get around this problem, Myers and his team designed their compound into a stiffened shape that closely resembles its binding target, giving it better grip on the ribosome. The researchers call their drug “pre-engineered” for ribosomal binding because it doesn’t need to expend as much energy to conform to its target as existing drugs have to do.
The researchers arrived at cresomycin using what they call component-based synthesis, a method developed by the Myers lab that involves constructing large molecular components of equal complexity and bringing them together at later stages, such as pre-building sections of a complex LEGO set before assembly. them. This fully synthetic, modular system allows them to manufacture and test not one, but hundreds of target molecules, significantly accelerating the drug discovery process.
The issues are clear. “Antibiotics are the foundation upon which modern medicine is built,” said co-author and graduate student Kelvin Wu. “Without antibiotics, many cutting-edge medical procedures such as surgeries, cancer treatments and organ transplants cannot be carried out.”
More information:
Kelvin JY Wu et al, An antibiotic prearranged for ribosomal binding overcomes antimicrobial resistance, Science (2024). DOI: 10.1126/science.adk8013. www.science.org/doi/10.1126/science.adk8013
Provided by Harvard University
Quote: Superbug killer: New synthetic molecule very effective against drug-resistant bacteria (February 15, 2024) retrieved February 15, 2024 from
This document is subject to copyright. Apart from fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.