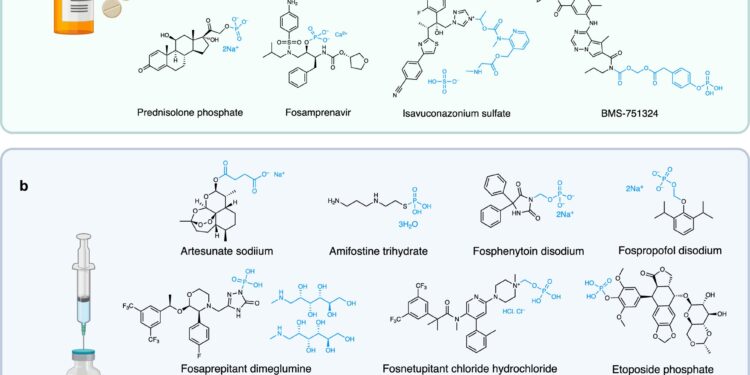
Examples of water-soluble prodrugs. A Orally administered medications that have a water-soluble property (e.g., a phosphate or phosphonooxymethyl group). b Commercial drugs administered intravenously with various water-soluble properties. Created in BioRender. Smith, M. (2024) BioRender.com/l22c048. Credit: Natural communications (2024). DOI: 10.1038/s41467-024-52793-6
For many people with cancer, intravenous (IV) chemotherapy infusions are the best chance for a cure. But these infusions can be inconvenient or inaccessible to patients, and some complications arise not from the active drug itself, but from the infusion. Turning these drugs into pills could be transformative.
In a study published in Natural communicationsA team of researchers led by Mark Smith, director of medicinal chemistry at Stanford University’s Sarafan ChEM-H, has designed a small molecular tag that, when added to almost any drug molecule, can make Medicines normally given intravenously are as effective as oral pills.
This also makes the pills more effective at lower doses. Through preliminary trials in mice, the team showed that their version of oral paclitaxel, one of the most prescribed chemotherapy drugs for many common cancers, worked better than the typical IV dose.
“This is an embarrassingly simple solution to an old problem,” Smith said. “With this strategy, we can accelerate the arrival of a wide variety of new drugs into the clinic.”
“The impact of a nontoxic and effective oral paclitaxel could be enormous,” said James Dickerson, a Stanford oncologist specializing in breast cancer care and health equity. Dickerson is not affiliated with the study. “This could lead to a better patient experience and, globally, it would increase access to care for patients with the most common cancers.”
Oil and water
A pill’s journey from the mouth to the bloodstream involves a few important steps. Once a person swallows a tablet, it dissolves in the stomach, releasing the drug molecules inside. These molecules are then absorbed by the walls of the stomach or intestines and end up in the bloodstream.
Once in the bloodstream, drug molecules can travel to the organs where they are needed. There, they pass through cell membranes and enter cells, where they finally get a chance to do the job they were designed to do. Often, drugs work by lodging into very specific pockets of particular proteins and preventing those proteins from carrying out a task.
To quantify how well a drug travels through the body, drug developers use the term “bioavailability,” which refers to the percentage of the total amount of drug you swallow that ends up in your bloodstream. It is normal that this figure is quite low, around 20%, but the reason may be surprising. This is because oil and water do not mix.
To complete the final stages of their journey – crossing cell membranes and inserting themselves into their protein pocket – many drugs must be lipophilic or oil-soluble. But to accomplish the first steps of the journey—formulating into a pill and dissolving in the stomach—the drug must be water-soluble. This is the central paradox of bioavailability: the drug must be soluble in both water and oil.
Sometimes a patient only needs a small amount of a particular drug in their blood to have an effect, so low water solubility is acceptable. But sometimes patients must meet a higher medical threshold. In these cases, they may need to take several pills several times a day, or take the medication through an IV infusion just to get enough in their blood.
A difficult pill to swallow
Most drug developers adopt one of two strategies to make oil-soluble drugs more water-soluble. In one strategy, they formulate the drug into a cocktail of other molecules. But scientists must adapt their “cocktail” to each new drug.
In a second strategy, they create a “prodrug,” which involves adding a small chemical tag to their drug molecule. The challenge is that the label must remain attached for just as long as necessary. If it drops too soon, the medicine will not be soluble in the stomach and will never be absorbed from the intestines. If the label never falls off, the drug will not be able to fit into its protein pocket.
Both of these strategies are complicated, time-consuming, and expensive, meaning scientists may have a molecule that could be transformative as a drug, but they will spend years of research trying to turn it into something a patient can swallow. .
Smith first discovered the problem when two clinicians contacted him the same week, frustrated that they could not dissolve two FDA-approved drugs in a liquid, which was a necessary step in their research. They needed Smith’s help.
Smith, who developed drugs at Roche before being recruited to lead Sarafan ChEM-H’s medicinal chemistry group in 2013, saw the potential to solve both laboratory inconveniences and the chronic clinical problem of low solubility of drugs. He thought he could develop a simple prodrug tag that would make any drug it was attached to soluble in water, and then drop at exactly the right time.
To do this, he designed the label to have the same chemical properties that allow soaps to cut fat, and he designed the label so that it would only be cleaved by the enzymes located at the top of the cells that line the stomach and intestines. Just when the prodrug is absorbed, the soap-like tag is ejected and the water-soluble prodrug changes to the oil-soluble drug.
He called this new label “ground and half” and he hoped that by hanging it on insoluble drugs he could make them effective in pill form.
Pass the test
One of the first drugs the team studied was vemurafenib, a highly water-insoluble melanoma treatment. This insolubility means patients have to take huge doses – four large tablets twice a day – and only a small amount is absorbed by the body. The solubility of the drug is so low that some patients do not respond to treatment at all.
The results were spectacular. Adding a sol moiety to vemurafenib caused the bioavailability to skyrocket from near zero to 100%. This means that adding a small chemical label could make the melanoma drug more effective for more patients, at a significantly lower dose.
“At the beginning of the project, we were just hoping to make the drugs water-soluble,” Smith said. “With this example, we went far beyond our expectations.”
The team then became more ambitious. Paclitaxel, often sold under the brand name Taxol, is one of the most widely prescribed chemotherapy drugs and is used to treat a variety of cancers, including breast, ovarian, and lung. More than a million patients have been treated with this drug over the past 30 years.
The drug is also almost completely insoluble in water and is only soluble in a mixture containing castor oil, meaning the drug can only be administered by IV infusion. But many patients experience adverse reactions to castor oil and therefore often need to be treated with an IV steroid infusion before the chemotherapy infusion which lasts several hours. The need for an IV drip also means patients must travel to a medical center for treatment, limiting global access to the drug.
An oral paclitaxel was the team’s ultimate test to evaluate its sol-fragment marker. In a mouse model of pancreatic cancer, modified oral paclitaxel, now water-soluble, performed better than a typical IV dose.
This is the first ever report of an effective oral prodrug to paclitaxel. Importantly, the researchers have so far not seen any toxicity associated with their sol-fragment label.
“This could transform the way millions of patients around the world receive chemotherapy,” Smith said. “They will have the convenience of staying at home to receive care, and they will not need to do long infusions or receive steroids.”
These results are still early and have only been tested in mice. Given the results so far, the team has high hopes that this could also improve the drug’s effectiveness in humans, while reducing treatment costs.
More information:
Arvin B. Karbasi et al, Sol-moiety: Discovery of water-soluble prodrug technology for enhanced oral bioavailability of insoluble therapeutics, Natural communications (2024). DOI: 10.1038/s41467-024-52793-6
Provided by Stanford University
Quote: New strategy could turn intravenous drugs into pills (October 8, 2024) retrieved October 8, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.