Credit: Cell Reports (2024). DOI: 10.1016/j.celrep.2024.114599
A new study published in Cell Reports Researchers at the Linda Crnic Institute for Down Syndrome (Crnic Institute) at the University of Colorado Anschutz Medical Campus report significant differences in oxygen physiology and red blood cell function in people with Down syndrome.
The study is part of the ongoing Human Trisome Project, a large and comprehensive cohort study of the Down syndrome population, including extensive annotation of clinical data, the largest biobank for the study of Down syndrome to date, and multi-omics datasets.
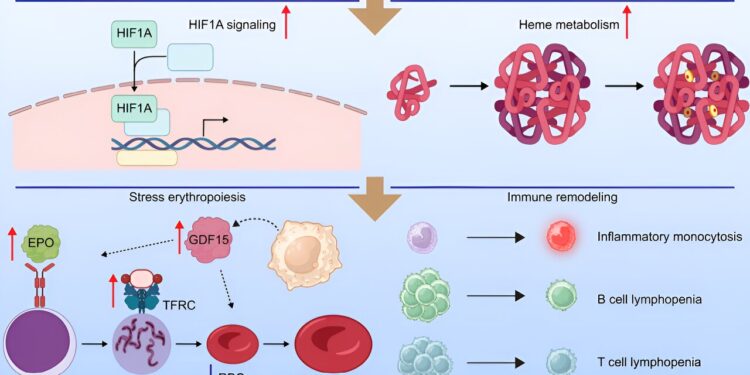
The Crnic Institute team first analyzed hundreds of blood samples to identify physiological differences between participants with Down syndrome and controls from the general population. They observed that triplication of chromosome 21, or trisomy 21, the chromosomal abnormality that causes Down syndrome, results in a physiological state reminiscent of hypoxia, or low oxygen supply.
They identified major changes in gene expression indicative of low oxygen availability, including the induction of many hypoxia-inducible genes and proteins, as well as increased levels of factors involved in the synthesis of heme, the molecule that carries oxygen inside red blood cells.
“These results reveal that hypoxia and hypoxic signaling should be at the forefront when we talk about the health of people with Down syndrome,” says Dr. Joaquín Espinosa, executive director of the Crnic Institute, professor of pharmacology, principal investigator of the Human Trisome Project and one of the study’s lead authors.
“Given the critical role of oxygen physiology in health and disease, we need to understand the causes and consequences of hypoxia in Down syndrome, which could lead to effective interventions to improve oxygen availability in this deserving population.”
“The results are remarkable. It’s safe to say that the blood of people with Down syndrome resembles that of someone who has been rapidly transported to high altitude or injected with erythropoietin (EPO), the master regulator of erythropoiesis, the process of forming new red blood cells,” said Dr. Micah Donovan, lead author of the study.
“Although it has been known for many years that people with Down syndrome have fewer and larger red blood cells, this is the first demonstration that they produce too much EPO and undergo stress erythropoiesis, a process in which the liver and spleen must start producing red blood cells to supplement those coming from the bone marrow.”
The team found that these phenomena are also observed in a mouse model of Down syndrome, reinforcing the idea that these important physiological changes result from the triplication of genetic material and the overexpression of specific genes.
“The fact that hypoxic signaling and stress erythropoiesis are conserved in the mouse model opens the door to mechanistic research that could identify the genes involved and reveal therapeutic interventions to improve oxygen physiology in Down syndrome,” said Kelly Sullivan, MD, associate professor of pediatrics, director of the experimental models program at the Crnic Institute and co-author of the study.
The research team also sought to determine whether elevated hypoxic signaling and associated stress erythropoiesis were linked to the heightened inflammatory state characteristic of Down syndrome. Although individuals with the strongest hypoxic signatures had more pronounced immune dysregulation and elevated inflammatory markers, their results indicate that reducing inflammation alone is not enough to reverse the hypoxic state.
“We will need much more data to understand what causes the hypoxic state and its impacts on the health of people with Down syndrome,” said Dr. Matthew Galbraith, assistant research professor of pharmacology, director of the data science program at the Crnic Institute and one of the paper’s senior authors.
“The hypoxic state could be caused by obstructive sleep apnea (which is common in Down syndrome), cardiopulmonary dysfunction, or perhaps even defects in red blood cell function. We are very excited about several ongoing clinical trials (…) on obstructive sleep apnea in Down syndrome, which we believe will be very informative.”
The Crnic Institute study team is already planning several follow-up studies, with the explicit goal of informing strategies to improve oxygen physiology in the Down syndrome population.
“This is another major advance from our scientists at the Crnic Institute that we hope will quickly lead to additional treatments,” said Michelle Sie Whitten, president and CEO of the Global Down Syndrome Foundation, a partner and affiliate of the Crnic Institute.
“As the mother of a bright 21-year-old with Down syndrome, I am eager to understand how to safely normalize oxygen physiology and how this can improve the lives of millions of people with Down syndrome around the world.”
More information:
Micah G. Donovan et al., Multimodal analysis of dysregulated heme metabolism, hypoxic signaling, and stress erythropoiesis in Down syndrome, Cell Reports (2024). DOI: 10.1016/j.celrep.2024.114599
Provided by CU Anschutz Medical Campus
Quote:New research reveals differences in oxygen physiology in people with Down syndrome (2024, August 15) retrieved August 15, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.