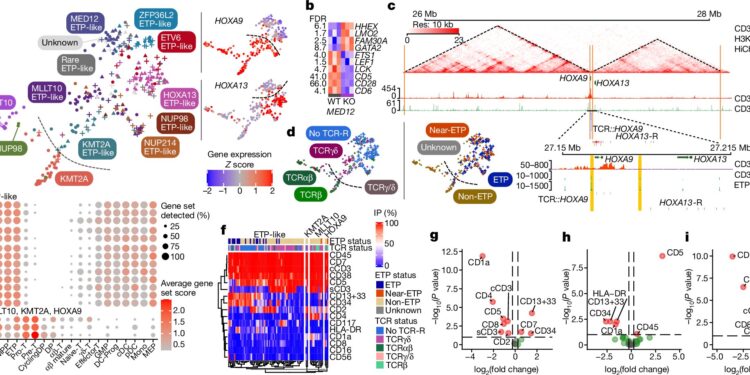
Genomic classification of ETP/ETP-like ALL. Credit: Nature (2024). DOI: 10.1038/s41586-024-07807-0
Researchers from Children’s Hospital of Philadelphia (CHOP), St. Jude Children’s Research Hospital (St. Jude) and Children’s Oncology Group (COG) today announced a significant paradigm shift in understanding T-cell acute lymphoblastic leukemia (T-ALL), an aggressive, high-risk form of cancer, to a form frequently caused by genetic changes in non-coding parts of our DNA.
The collaborative study was published today in the journal Nature.
Many children, adolescents, and young adults with T-ALL typically respond well to initial treatment. However, patients who relapse or develop treatment-resistant disease often face a poor prognosis. Given the aggressive nature and rapid progression of the disease, as well as the limited understanding of the genetic basis of T-ALL, researchers have identified an urgent need for new, effective approaches to diagnosis and treatment.
“This paper is the first to transcend previous barriers and comprehensively profile the entire genome, revealing critical information about more than 1,300 children, adolescents and young adults with T-ALL,” said David T. Teachey, MD, attending physician, director of clinical research at CHOP’s Childhood Cancer Research Center and chair of the COG Acute Lymphoblastic Leukemia Committee.
“These results represent a significant clinical advance, as the goal of treating T-cell chronic lymphocytic leukemia is to prevent relapse, which requires identifying patients at highest risk. These data now make it possible to risk-stratify patients with T-cell leukemia, identifying those at high risk of relapse so that they can be treated with newer or alternative drugs.”
Previous studies have failed to identify significant genetic changes in T-ALL because they have focused on the coding genome, the part of DNA that encodes proteins, the building blocks of cells. However, only 1% of DNA is coding, while the remaining 99% is called noncoding.
Once thought to be useless, the noncoding region now plays a key role in regulating biological processes. It tells the cell when to produce certain proteins, like a crossing guard that helps people cross the street safely.
In this case, the researchers studied more than 1,300 patients treated in the COG AALL0434 clinical trial and sequenced each patient’s tumor and non-tumor genomes. While researchers previously suspected that non-coding DNA in T-ALL played an important role, the results of this study are the first to establish this fact on a large scale.
The study found that approximately 60 percent of the genetic changes that drive T-ALL cancer cells are noncoding changes. This fundamentally changes the way researchers think about T-ALL, providing a deeper understanding of the biology of the disease. This is leading to innovative treatments, including new immunotherapies being developed at CHOP and St. Jude.
Traditionally, patients with T-ALL are classified according to their risk based on their response to treatment and their immunophenotype, which is used to profile cell surface proteins as part of the diagnostic workup. Although cell surface protein expression helps define T-ALL subtypes, it has not been shown to consistently identify patients with a good prognosis.
The new comprehensive data revealed why, strongly suggesting that a genomic approach should replace current immunophenotypic classification. Accordingly, the researchers developed models that integrate genetics and treatment response to accurately stratify the risk of T-ALL patients and are currently validating the results using patient samples from the upcoming COG T-ALL trial.
“It was striking how many of these noncoding changes there were and how many of them were enhancer disruption events, whether it was the hijacking or co-optation of an existing enhancer, or changes that generated a new enhancer,” said Charles Mullighan, MBBS, MD, St. Jude Children’s Research Hospital, deputy director of the Comprehensive Cancer Center and member of the Department of Pathology.
“We now have a much stronger framework to bring these alterations back to the lab and say we have better information to build the right models to understand the biology and then test the therapy. We have very clear information about the types of alterations that people should focus on to create a diagnostic test.”
The researchers were able to classify T-ALL into 15 subtypes with distinct gene expression and genomic factors, including previously undefined subtypes. They refined the classification of known subtypes and showed that motor lesions, other genetic changes, and cell type of origin work together to define the genomic subtype and the clinical and biological features of a disease.
They also observed a significant link between the type of genetic alterations and the outcomes of T-ALL. This new observation shows that it is not only the gene altered in cancer cells, but also the way in which it is altered, that helps define the prognosis and chances of cure.
“Future research must continue to determine broader applications for this approach,” Teachey said. “These results provide a strong roadmap to improve patient outcomes and cure more children and adults with T-ALL.”
More information:
Petri Pölönen et al., The genomic basis of childhood T-cell acute lymphoblastic leukemia, Nature (2024). DOI: 10.1038/s41586-024-07807-0
Provided by St. Jude Children’s Research Hospital
Quote:New research poised to transform approach to diagnosis and treatment of acute leukemia in children (2024, August 14) retrieved August 14, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.