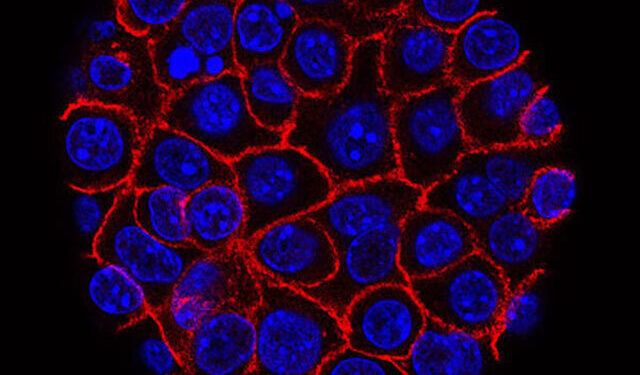
Pancreatic cancer cells (blue) growing into a sphere surrounded by membranes (red). Credit: National Cancer Institute
Researchers from the University of Massachusetts Amherst and UMass Chan School of Medicine have demonstrated a new method in mice to fight pancreatic cancer. The study, published in Scientific translational medicinedescribes the synergistic effects of a novel nanoparticle-based drug delivery system to activate an immune pathway in combination with tumor-targeting agents.
Pancreatic ductal adenocarcinoma (PDAC) is the most common form of pancreatic cancer. With a five-year survival rate of 13%, it is the third leading cause of cancer death.
One of the main challenges is the microenvironment surrounding the tumor. This environment is characterized by dense tissue creating a barrier around the tumor that inhibits blood vessel formation and blocks immune infiltration.
“Drug delivery is a huge challenge because of the architecture of the microenvironment of these hard-to-treat tumors,” says Prabhani Atukorale, assistant professor of biomedical engineering at UMass Amherst and one of the study’s corresponding authors. She adds that the environment also blocks the body’s immune cells from activating and entering the tumor.
“Pancreatic cancer, unfortunately, does not respond to most conventional therapies like chemotherapy, or even immunotherapy, which has revolutionized many cancer therapies in the last 10 years,” said Marcus Ruscetti, assistant professor of molecular, cellular and cancer biology at UMass Chan Medical School, and another corresponding author.
Ruscetti’s previous research has shown that two cancer drugs (trametinib, a MEK inhibitor, and palbociclib, a CDK4/6, or T/P, inhibitor) can promote the development of blood vessels, allowing T cells (and chemotherapy) to penetrate the tumor more easily. However, the cancer “tricks” the immune system into thinking the tumor is just a normal, healthy clump of cells. Because the T cells aren’t activated, simply having more of them won’t eliminate the cancer.
This is where the researchers want to implement a trick of their own. The first pathway is called the Stimulation of Interferon Genes (STING) pathway. STING recognizes viral infections in the body.
“If we can trick the immune system into thinking it’s a viral infection, then we’re harnessing a very robust anti-tumor immune response to mount tumor immunotherapy,” Atukorale says.
The researchers also wanted to activate the TRL4 pathway, because it enhances the effects of STING activation. They used agonists, which are chemicals that can trigger a biological response; in this case, in immune-stimulating pathways. But getting these immune-triggering chemicals through the tumor microenvironment remains a challenge.
The researchers’ solution: encapsulate the STING and TRL4 agonists in a novel lipid-based nanoparticle design. Nanoparticles have several advantages. First, research has shown that they are highly effective at introducing agonists into the challenging tumor microenvironment.
The design also allows the two agonists to be combined, which is a challenge since the two agonists mix as well as oil and water. “This ensures that they are transported together in the bloodstream, reach the same target cell together, and are taken up by the same target cell together,” Atukorale says.
“We use lipid-based biocompatible materials to encapsulate drugs that functionally work together but don’t like to be next to each other, and then we’re able to use engineering capabilities to integrate various functionalities to direct them where they need to go,” she says.
The synergistic effect of the two agonists and T/P therapy proved effective: eight out of nine mice had their tumors necrotize and shrink. “We also had two mice that had a complete response, meaning the tumors completely disappeared, which is quite striking,” Ruscetti says. “We had never seen that in this model before.”
There is still work to be done because the tumors returned after the mice stopped treatment, but Ruscetti says this remains a very encouraging step toward a cure.
“If you’re going to attack other types of cancer besides pancreatic cancer, you need a combination therapy that targets the tumor and the immune system,” he adds. “This is a strategy that can do that.”
Treatments for cancers like PDAC that could be derived from this study include mutations in colon cancer, lung cancer, liver cancer and cholangiocarcinoma (bile duct cancer).
Prabhani adds that the modular nature of this design allows for therapies that are easily customizable for patients. “It’s kind of plug and play,” she says.
“We can tailor the agonist ratios, the drug combinations, the targeting molecules, while keeping essentially the same platform. That’s what will hopefully enable translational application, but also tailoring to individual patients, because many of these cancer therapies need to be personalized.”
Finally, she applauds the power of collaboration between the two UMass institutions, saying, “This kind of system is easy to build when you have complementary, but multidisciplinary and interdisciplinary, expertise.”
More information:
Loretah Chibaya et al, Administration of innate immune agonist nanoparticles combined with senescence-inducing agents promotes T cell control of pancreatic cancer, Scientific translational medicine (2024). DOI: 10.1126/scitranslmed.adj9366. www.science.org/doi/10.1126/scitranslmed.adj9366
Provided by the University of Massachusetts Amherst
Quote:New pancreatic cancer treatment proves effective in shrinking and eliminating tumors (2024, August 28) retrieved August 28, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.