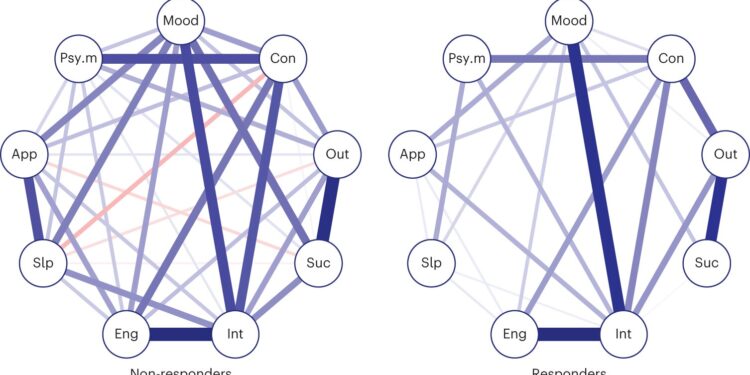
The connectivity strength of the symptom network is weaker in responding patients than in non-responding patients. Network structures of non-responders (n = 1,907) and responders (n = 637) at baseline. Blue connections represent positive associations, while red connections represent negative associations. Thicker edges represent stronger associations (both positive and negative). Psy.m, psychomotor agitation; Disadvantage, concentration/decision making; Mood, depressed mood; Eng, fatigue or loss of energy; Slp, sleep problem (falling asleep, middle, early insomnia and hypersomnia); Out, self-vision; Suc, suicidal ideation; Int, implication; Application, weight/appetite change. A network comparison test was used to compare the groups. ***P-value = 0.004. Credit: Natural mental health (2024). DOI: 10.1038/s44220-023-00192-z
Surveys and statistics suggest that mental illnesses are increasingly prevalent, as the number of people seeking mental health services around the world has increased in recent years. Understanding the factors that may predict well-being and contribute to recovery from mental health disorders is therefore of utmost importance, as it could inform the development of new therapeutic interventions.
Researchers at the Istituto Superior di Sanita recently set out to explore the role of plasticity, the brain’s ability to change in response to new experiences and environmental factors, in healing depression. Their article, published in Natural mental healthpresents results from an in-depth network analysis of data on depressed patients, which could inform the work of psychiatrists and mental health professionals.
This research group has been carrying out studies focused on the plasticity of the human brain for some time now. Their recent work adopts a so-called network perspective; an emerging approach in psychology research that views mental health disorders as networks.
“We worked with antidepressants and selective serotonin reuptake inhibitors (SSRIs) and found that, as a growing number of studies show, these drugs have a strong effect on plasticity,” said Igor Branchi, co-author of the article, to Medical Xpress. . “These drugs increase plasticity and make patients more susceptible to changes in mood and mental health. Once a patient is more plastic and more susceptible to change in mood, it is the environment that can play a role. key role.”
Many recent studies have investigated the impact of brain plasticity on mental health. Branchi and colleagues hypothesized that while plasticity itself is neither good nor bad, when combined with a supportive environment, it can predict the transition from depression to mental health.
“You could think of plasticity as the door to a room, where being in the room represents being sick, and the outside of the room being healthy,” Branchi explained. “In this metaphor, increasing plasticity is like opening the door, although it doesn’t push me out of my room, it allows me to get out of the room. What pushes me out of the room is usually something else , generally associated with the individual’s context, which includes both objective characteristics of the environment and subjective evaluation.
Looking at plasticity from this perspective, identifying a strategy to reliably measure it could be greatly beneficial, as it could help to better understand the factors contributing to poor mental health in individual patients. By determining whether patients exhibit little neuroplasticity or whether their brains easily adapt based on their experiences, psychiatrists may be able to design more effective treatment strategies.
The recent study by Branchi and colleagues draws on recent studies that examine mental health from a network perspective. Network theories of psychopathology view mental health disorders as networks, with symptoms as nodes and the relationship between them represented by the connections between these nodes.
“In these networks, the nodes are the symptoms, while the connections between the nodes characterize how these symptoms correlate with each other,” Branchi said. “If they are correlated with each other, that means they are happening at the same time.”
In the context of this study, plasticity implies a weaker correlation between different symptoms, whereas no plasticity results in a stronger correlation. Branchi and colleagues analyzed one of the largest datasets published to date, the STAR*D dataset published by the National Institute of Mental Health (NIMH) in the United States.
“STAR*D is a large dataset that was developed to study therapeutic alternatives to treat depressed patients,” Branchi said. “In our study, we leveraged this dataset from a completely different perspective than its original purpose, looking at recorded patient symptoms and the perceived quality of their environment.”
The researchers also took into account subjective responses to a survey designed to measure participants’ overall life satisfaction. This is important because different individuals may view their lives in a more optimistic or pessimistic light, regardless of their objective socioeconomic status and environmental context.
“We then used the symptoms recorded in the dataset to build a network,” Branchi explained. “We also looked at how much they had improved after the four-week intervention period. It is important to say that we selected patients with the same baseline level, to ensure that patients who had improved improved and those who did not improve started from the same point.
The analysis by Branchi and colleagues yielded some interesting results, ultimately suggesting that the mental health of patients who had greater neuroplasticity at baseline (i.e., those whose symptoms were weakly correlated) had improved. improved further over time. Overall, this hints at the potential value of network theories of psychopathology in predicting the plasticity of individuals.
“Our results suggest that the improvement observed in patients is also associated with the quality of their environment,” Branchi said. “That’s why we don’t measure improvement, but plasticity. In other words, we measure how much a person is likely to change in a favorable environmental context.”
Recent work from this research group hints at the potential value of network theories as tools to operationalize plasticity in research and clinical settings. While Branchi and colleagues specifically focused on recovery from depression, their approach could soon be applied to other mental health disorders characterized by multiple interacting symptoms, such as anxiety disorders, bipolar disorder, and more.
“The strategy we have developed allows for a stratification of patients between those who are already plastic and could thus benefit most from psychotherapy and positive life changes, and others who already live in a supportive environment but are stuck in a depressive state.
“It is likely that this second type of patient would benefit first from an intervention designed to increase plasticity and susceptibility to change, such as pharmacological treatments that increase neuroplasticity.
“There is also a third type of patients who live in unfavorable conditions and are not plastic, so they would probably need both psychotherapy and pharmacological treatment. A fourth type, who already lives in an environment favorable and who is already plastic, could benefit from different therapies. approaches.”
By dividing patients based on these factors, clinicians might be able to introduce carefully tailored treatments that might yield more positive results. Although the recent paper by Branchi and colleagues does not provide specific medical advice, it could inform the work of mental health practitioners, offering a new way to predict a patient’s plasticity.
“From a philosophical point of view, our study suggests that in a networked system, plasticity arises from the interaction between different nodes,” Branchi added. “So there is no process behavior associated with plasticity, but rather plasticity arises from the interaction between different symptoms, behaviors or elements. This is something that we think could be very conceptually important.”
More information:
Toward a network operationalization of plasticity to predict the transition from depression to mental health. Natural mental health(2024). DOI: 10.1038/s44220-023-00192-z.
© 2024 Science X Network
Quote: Network analysis highlights key role of plasticity in transition from depression to mental health (February 20, 2024) retrieved February 20, 2024 from
This document is subject to copyright. Apart from fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.