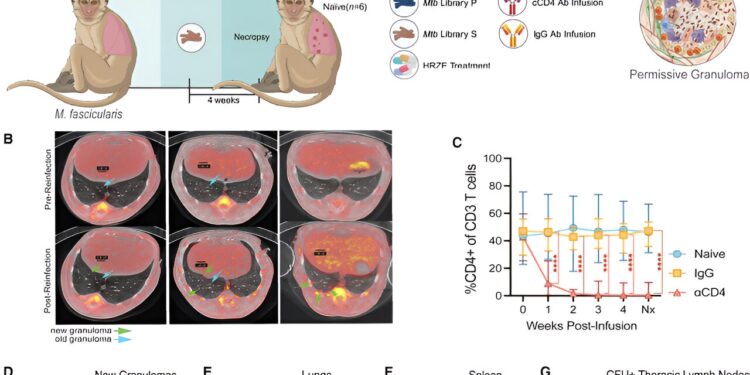
Anti-CD4 antibody infusion depleted CD4+ T cells in anatomical compartments in cynomolgus macaques. Credit: Immunity (2024). DOI: 10.1016/j.immuni.2024.08.002
The body’s first line of defense against tuberculosis (TB) involves immune cells that suppress lung inflammation instead of activating it, report scientists from the University of Pittsburgh and the Ragon Institute at Massachusetts General, MIT and Harvard. Immunity.
Research has shown that a subset of infection-fighting white blood cells, called CD4 T cells, protect the lungs from reinfection by creating an anti-inflammatory environment in lung tissue, rather than by secreting molecules that directly kill the invading bacteria Mycobacterium tuberculosis, or Mtb, that causes tuberculosis.
This unexpected discovery complements previous research on the role of protective immune T cells in controlling TB infection and points to ways to improve existing TB vaccines.
“Our study suggests that a vaccine that induces the ‘right’ type of CD4 T cells that rapidly limit inflammation upon infection could be critical to providing long-lasting immunity,” said senior and corresponding author JoAnne Flynn, Ph.D., distinguished professor and chair of microbiology and molecular genetics at Pitt.
Although TB has been virtually eradicated in the United States, an estimated 10.6 million people worldwide were infected with the disease in 2022. TB remains particularly prevalent and deadly in Southeast Asia, Africa, and the Western Pacific, where epidemics occur regularly and people are often exposed to Mtb multiple times, even after recovery from the initial infection.
Mtb infection is often accompanied by symptoms such as persistent cough, extreme exhaustion, and fever, and can cause lung inflammation and scarring. Yet, despite its significant public health burden, the disease has not yet been eradicated, largely because of the relative ineffectiveness of the existing vaccine, bacille Calmette-Guérin (BCG), which can protect young children but not adults.
The development of better vaccines has been limited by an imperfect understanding of the dynamic interaction between Mtb and the host immune system and how Mtb evades the immune response.
In humans, prior Mtb infection confers some level of protection against developing TB after re-exposure. To better understand the effect of prior infection on subsequent Mtb infections, Flynn and his team turned to macaques that had been exposed to the pathogen in the past. Flynn’s previous research has shown that ongoing or drug-treated TB protects against re-infection and disease. In the new study, the researchers investigated whether CD4 T cells are critical to this protection.
Surprisingly to Flynn, instead of seeing CD4 T cells secrete molecules that attracted other infection-fighting cells to sites of Mtb invasion, the CD4 cells instead contained the inflammation, making the site of infection less hospitable to the bacteria.
Using precise molecular techniques, including single-cell RNA sequencing, the team showed that this process is mediated in part by the effects of CD4 T cells on CD8 T cells, another subset of immune white blood cells whose primary function is to kill cells infected with viruses.
This interaction between CD4 and CD8 cells that Flynn observed while studying Mtb reinfection complements his previous research that suggested that CD8 T cells control Mtb infection by creating an anti-inflammatory environment in the lung.
The researchers concluded that the interaction between CD4 and CD8 T cells creates an anti-inflammatory environment hostile to Mtb and, therefore, limits bacterial growth and disease severity.
A better understanding of the role of CD4 T cells in preventing tuberculosis could provide new strategies for vaccine development.
“Our work demonstrates that controlling TB requires a complex and sophisticated interplay of immune factors,” Flynn said. “Vaccine strategies have focused on inducing inflammatory CD4 T cells, but it may be time to shift our focus to reducing inflammation to the minimum level needed to limit bacterial growth, which will involve using anti-inflammatory CD8 T cells and other cell types early in the course of infection.”
More information:
Joshua D. Bromley et al, CD4+ T cells rewire granuloma cellularity and regulatory networks to promote immunomodulation after Mtb reinfection, Immunity (2024). DOI: 10.1016/j.immuni.2024.08.002
Provided by the University of Pittsburgh
Quote:Immune protection against tuberculosis reinfection is provided by cells that dampen lung inflammation, study finds (2024, August 29) retrieved August 29, 2024, from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.