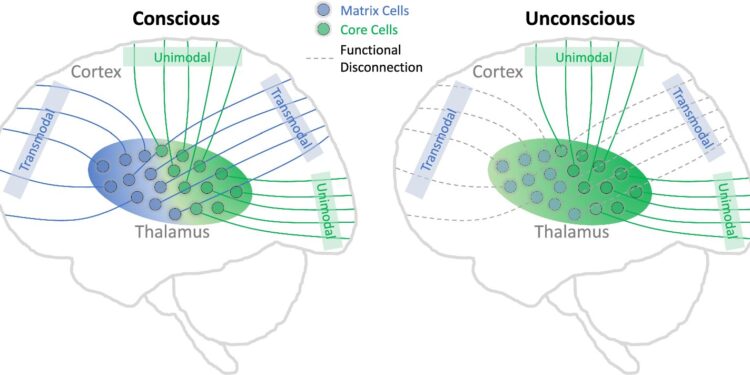
Schematic illustration of the main conclusion. Credit: Nature Communications (2024). DOI: 10.1038/s41467-024-51837-1
In hospital operating rooms and intensive care units, propofol is a drug of choice, widely used to sedate patients for comfort or render them completely unconscious for invasive procedures.
Propofol acts quickly and is well tolerated by most patients when administered by an anesthesiologist. But what happens inside the brain when patients are asleep, and what does it reveal about consciousness itself?
UM researchers studying the nature of consciousness have successfully used the drug to identify the complex brain geometry behind the unconscious state, providing unprecedented insight into brain structures that have traditionally been difficult to study.
“Consciousness has been studied from many different perspectives, and understanding the neurobiological underpinnings of consciousness has major implications for multiple medical disciplines such as neurology, psychiatry and anesthesiology,” said Zirui Huang, Ph.D., assistant research professor in the Department of Anesthesiology at UM Medical School.
Until now, researchers have debated how anesthetics suppress consciousness. Specifically, they have wondered whether their site of action is primarily in the thalamus, an egg-shaped structure deep in the brain that receives information from what we see, touch, and hear, or in the cerebral cortex, which processes this information in complex ways.
A study published in the journal Nature Communications and led by Huang, George Mashour, MD, PhD, and Anthony G. Hudetz, PhD, of the UM Center for the Science of Consciousness, describes for the first time in humans how connections between brain cells in these two important areas are altered by propofol. The paper is titled “Propofol Disrupts the Functional Architecture of the Human Central Thalamic Matrix.”
In healthy volunteers, they mapped changes in brain architecture before, during, and after propofol sedation, guided by functional magnetic resonance imaging (fMRI). This allowed them to monitor blood flow to areas of the brain as study participants entered and exited a state of unconsciousness.
Initially, Huang explains, the thalamus has a balanced level of activity between both specific nuclei (groups of brain cells) that send sensory information to highly defined areas of the cortex—known as unimodal processing—and nonspecific nuclei that send information more diffusely across a higher layer of the cortex, known as transmodal processing.
The team found that under deep sedation, the thalamus showed a drastic reduction in activity in the groups of brain cells responsible for transmodal processing, leading to a dominant unimodal pattern, suggesting that although sensory inputs are still being received, there is no integration of these inputs.
“The field has been focused on anesthetic effects on the thalamus and cortex for more than two decades. I think this study advances neurobiology significantly,” said George Mashour, MD, PhD, professor of anesthesiology and pharmacology and founder of the UM Center for Consciousness Science.
Next, they discovered the specific cell types that played a role in the shift to an unconscious state and their relationship to the change in thalamic processing. The thalamus contains at least two distinct cell types, Huang said, core cells and matrix cells.
“We now have compelling evidence that widespread connections of thalamic matrix cells with higher-order cortex are essential for consciousness,” says Hudetz, a professor of anesthesiology at UM and current director of the Center for the Science of Consciousness.
Thinking of the cortex as layered like an onion, core cells connect to lower layers while matrix cells connect to upper layers in a more spread-out manner.
By measuring mRNA expression signatures, like cell identification badges, they were able to see that disruption of matrix cell activity played a more important role in the transition to unconsciousness than central cells. Another surprise was that GABA, a major inhibitory transmitter in the brain generally thought to be essential to propofol’s actions, did not appear to play as large a role as expected.
“The results suggest that loss of consciousness during deep sedation is mainly associated with functional disruption of matrix cells distributed throughout the thalamus,” Huang said.
More information:
Huang, Z., et al. Propofol disrupts the functional architecture of the central thalamic matrix in humans. Nature Communications (2024). DOI: 10.1038/s41467-024-51837-1
Provided by the University of Michigan
Quote:How the Brain’s Inner Chamber Regulates Our Consciousness (2024, September 9) retrieved September 9, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.