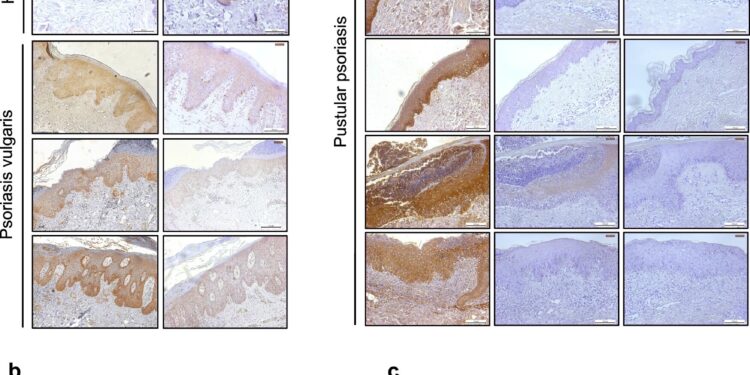
Analysis of hepcidin expression in patients with psoriasis. Credit: Natural communications (2024). DOI: 10.1038/s41467-024-50993-8
Scientists may have discovered the root cause of psoriasis, a chronic and sometimes debilitating skin disease that affects 2 to 3 percent of the world’s population. The disease is characterized by red, scaly patches that impact the patient’s quality of life and can sometimes be life-threatening.
New research strongly suggests that the hormone hepcidin may trigger the onset of the disease. This is the first time that hepcidin has been considered as a potential causative factor. In mammals, hepcidin is responsible for regulating iron levels in the body.
The study is published in the journal Natural communications.
The international research team behind this discovery, which includes Dr Charareh Pourzand from the Department of Life Sciences, Center for Therapeutic Innovation and Center for Bioengineering and Biomedical Technologies at the University of Bath, hopes that their findings will lead to the development of new drugs capable of blocking the action of the hormone.
The patients most likely to benefit from such treatment are patients with pustular psoriasis (PP), a particularly severe and treatment-resistant form of the disease that can affect the nails and joints as well as the patient’s skin.
Dr Pourzand, who studies ways to alleviate iron imbalances in the skin, said: “Psoriasis is a life-changing dermatological disease. Patients face a potentially disfiguring and lifelong affliction that profoundly affects their lives, causing both physical discomfort and emotional distress. This disease can also lead to other serious health problems.
“A new treatment targeting the imbalance of iron hormones in the skin offers hope. This innovative approach could significantly improve the quality of life of millions of people, restoring their confidence and well-being.”
We need iron for the skin, but not too much
Iron is an essential trace metal, not only for carrying oxygen through the body’s circulatory system, but also for maintaining healthy skin. It is involved in many essential cellular functions, including wound healing, collagen production and immune function. However, iron overload in the skin can be harmful, amplifying the damaging effects of the sun’s UV rays and causing chronic hyperproliferative diseases (where cells grow and multiply more than normal), including psoriasis.
Studies going back 50 years have reported elevated iron concentrations in the skin cells of psoriatic patients. However, the cause of this excess and its importance for the disease remain unclear until now.
The new study is the first to name hepcidin as a likely link.
Hepcidin is responsible for controlling the amount of iron absorbed from food and then released into the body. In healthy individuals, it is produced exclusively in the liver. However, the new study found that in people with psoriasis, the hormone is also generated in the skin.
Hepcidin exposure triggers iron overload
In the new study, mice (which have many genetic and physiological similarities to humans) developed a rodent form of psoriasis after being exposed to high levels of hepcidin produced by the skin.
This overabundance of the hormone caused the animals’ skin cells to retain much more iron than necessary. In turn, this excess iron triggered both hyperproliferation of skin cells and an abnormally high concentration of inflammation-inducing neutrophils (a type of immune system cell) in the upper layer of the skin.
These two findings – an overproduction of skin cells and an abundance of neutrophils – are the main characteristics of human psoriasis.
Psoriasis is hereditary, although experts believe that “environmental” factors such as weight, infections and smoking are also triggers.
A disease without a cure
There is currently no cure for psoriasis, although treatments including topical creams, light therapy and oral medications can help control symptoms in patients with some forms of the disease. Recent treatments have focused on targeting immune pathways that contribute to the development of psoriasis.
Dr. Pourzand believes that a drug targeting hepcidin has the potential to significantly improve treatment options for all psoriasis patients.
She said: “Our data strongly suggest that hepcidin would be a good target for the treatment of cutaneous psoriasis. A drug that can control this hormone could be used to treat flare-ups and keep patients in remission to prevent recurrences.
“Additionally, by adjusting excess iron in psoriatic skin with personalized iron chelators (substances that bind to excess iron in the body and help remove it), we will aim to stop uncontrolled overgrowth psoriatic skin cells. This hyperproliferation is a major objective of our laboratory’s research on the treatment of psoriasis, carried out in collaboration with national and international scientists from the Skin@Bath network, including those in this study.
Dr William Tillett, senior lecturer at the University of Bath and consultant rheumatologist specializing in the diagnosis and treatment of psoriatic arthritis, said: “This research by Dr Pourzand and colleagues is an exciting step forward for people living with psoriasis and for the clinical teams who care for them.
“We don’t know exactly why people develop psoriasis, but identifying hepcidin as an important factor in the development of the disease opens the door not only to potential new treatments, but also to the possibility of preventing the development of the disease in people at high risk Existing drugs, called biologics, can be very effective, but they are expensive and rationed in the UK. Additionally, these drugs do not work for everyone and may stop working. function after a certain time. A new therapeutic approach would therefore be very useful.
He added: “However, drug development is notoriously time-consuming and expensive, so a new treatment will not be available immediately and it is important that patients manage their expectations.”
Dr Penelope Pratsou, consultant dermatologist and spokesperson for the UK charity British Skin Foundation, said: “The results of this study shed new light on the pathophysiology of psoriasis, with the overabundance of hepcidin in psoriatic skin being considered another culprit. appear promising for patients, although additional research is needed to further elucidate the role of hepcidin and its potential as a potential psoriasis treatment target.
More information:
Elise Abboud et al, Cutaneous hepcidin initiates psoriasiform skin inflammation via Fe-induced hyperproliferation and neutrophil recruitment, Natural communications (2024). DOI: 10.1038/s41467-024-50993-8
Provided by the University of Bath
Quote: Faulty iron hormone in the skin may cause psoriasis (September 26, 2024) retrieved September 26, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.