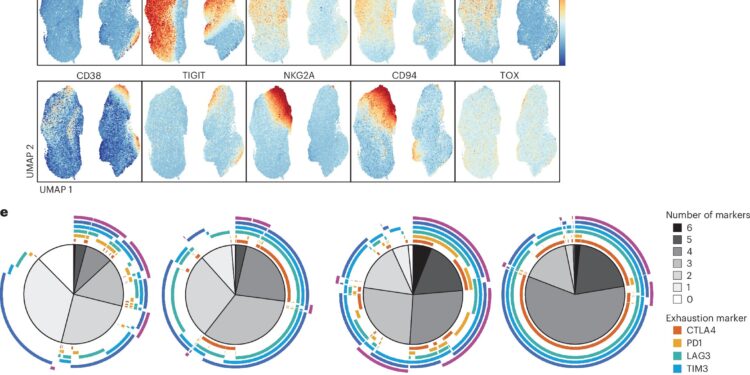
Exposure of AML to cytokines results in depletion of CART-123. Credit: Natural medicine (2024). DOI: 10.1038/s41591-024-03271-5
In the clinical battle against leukemia, recent breakthroughs in chimeric antigen receptor T (CAR T) cells have given patients and physicians an unprecedented weapon. CAR T cell therapy has demonstrated efficacy in the treatment of B-cell malignancies, achieving high response rates and durable remissions. However, translating this success to acute myeloid leukemia (AML) has proven difficult.
Researchers at the University of Pennsylvania studied the use of patient-derived anti-CD123 CAR T cells in the treatment of adults with relapsed or refractory AML. They detail their findings in a paper titled “Cytokine-Mediated CAR T Therapy Resistance in AML,” published in Natural medicine.
Although the therapy was successfully administered to most participants, results highlighted significant challenges related to cytokine release syndrome (CRS) and relatively low clinical response rates. This suggests that combining CAR T cell therapies with cytokine signaling inhibitors could improve treatment outcomes for AML patients.
CAR T cells are created from a patient’s own T cells. T cells are collected and engineered in the laboratory to produce synthetic proteins on their surface (chimeric antigen receptors). These proteins recognize and bind to specific proteins, or antigens, on the surface of cancer cells.
Before being reinjected into the patient, the CAR T cells are multiplied by the millions, giving them a good starting advantage. The CAR T cells will continue to multiply in the patient’s body and, through new receptors, will be able to identify and kill cancer cells carrying the targeted antigen on their surface throughout the body.
AML is aggressive and there are few effective treatment options for relapsed or refractory cases. Despite advances in therapeutic strategies, outcomes for these patients remain poor. Previous studies have noted that AML cells frequently express a protein called CD123 and associated it with poor prognosis.
Preclinical studies have suggested that CAR T cells targeting CD123 (CART-123) may be effective. The current study evaluates the safety and efficacy of CART-123 in adult patients with relapsed or refractory AML.
The study enrolled 22 patients, of whom 20 were confirmed eligible. The median age of participants was 60 years. CART-123 cell manufacturing was successful in 90.4% of attempts, achieving a median T cell purity of 98.5%. All patients received standard lymphodepletion conditioning treatment with fludarabine and cyclophosphamide before CART-123 infusion.
Of the six patients evaluated for response, two achieved a complete molecular response, one achieved a measurable complete response to residual disease with incomplete hematologic recovery, and three had stable or progressive disease.
The overall response rate was 25%. The median duration of remission for these responding patients ranged from 84 to 381 days, with a median overall survival after infusion of 160 days.
CRS was a significant adverse event, occurring in 83% of patients, with severe cases resulting in dose-limiting toxicity and death in two individuals.
The analysis revealed that myeloid-supportive cytokines such as IL-3, GM-CSF, and FLT3L were secreted during CART-123 treatment, promoting the survival of AML bursts via kinase signaling. This cytokine activity essentially reduced the sensitivity of AML cells to the specifically designed CART-123.
These findings are consistent with established knowledge that myeloid-supportive cytokines are linked to chemoresistance in AML, and previous studies have associated these cytokines with higher relapse rates and poorer overall survival in AML.
The research team reasoned that blocking the JAK/STAT signaling pathway with ruxolitinib could restore the sensitivity of AML cells to CART-123, suggesting that combination therapies could improve treatment effectiveness.
They tried it and it worked.
Blocking cytokine signaling with the JAK1/2 inhibitor ruxolitinib restored the efficacy of CART-123 against AML. The researchers conclude that their results may not be limited to CART-123 therapy alone, suggesting that other methods of immunotherapy may be weakened by the same cytokine pathways found in their study.
According to the article’s conclusion, “our study thus illuminates a blind spot in previous immunotherapy studies directed against AML and provides strong arguments in favor of combination therapies involving CAR T cells and signaling blockade in the context of myeloid cancers.
More information:
Anand S. Bhagwat et al, Cytokine-Mediated CAR T Therapy Resistance in AML, Natural medicine (2024). DOI: 10.1038/s41591-024-03271-5
© 2024 Science X Network
Quote: Failed CAR T cell trial could unlock multiple treatments for acute myeloid leukemia (October 8, 2024) retrieved October 8, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.