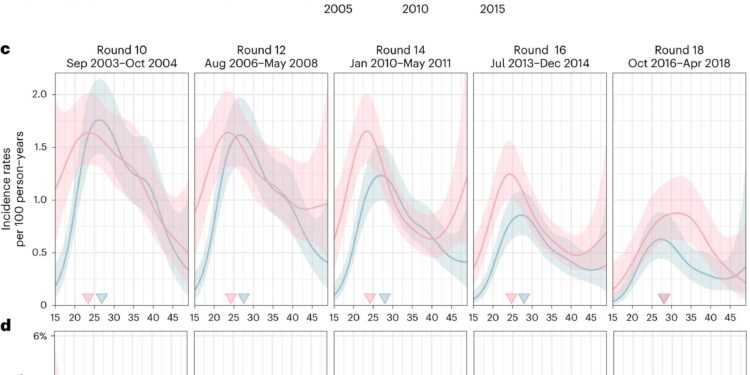
Temporal trends in age-specific HIV incidence rates among men and women in Rakai, Uganda. A,Location of RCCS in south-central Uganda. Survey results are reported for all RCCS communities located inland from Lake Victoria over nine survey cycles. bNumber of RCCS participants in the census-eligible population aged 15 to 49, by survey cycle. vsEstimated average HIV incidence rates per 100 years of exposure among uninfected individuals (row) by one-year age group, sex (colors) and survey cycle, as well as confidence intervals at 95% (ribbon) and the median age of incident cases (arrowhead). d, Estimated median contribution to incidence cases in the study population (row) by 1-year age group, sex (colors) and survey cycle, as well as 95% confidence intervals (ribbon). In all subfigures, incidence estimates are based on not = 1,117 individuals in the incidence cohort. Credit: Natural microbiology(2023). DOI: 10.1038/s41564-023-01530-8
A study spanning 15 years of HIV transmission and suppression in Uganda reveals how closing the gender gap in treatment could reduce infection rates.
Providing more heterosexual men with easy access to HIV treatment and care could help suppress the virus and quickly reduce transmission to their female partners, according to a new study published in Natural microbiology .
The research, led by scientists from Imperial College London and the Rakai Health Sciences Program (RHSP) in Uganda, analyzed 15 years of data from 2003 to 2018, during which the US President’s Emergency Plan for fight against AIDS (PEPFAR) has implemented a vast program. screening, prevention and treatment of HIV/AIDS.
This included the distribution of antiretroviral therapy (ART) drugs, which suppress the virus so that a person is no longer contagious. The analysis shows that the PEPFAR program and other services significantly reduced new infections among young women and heterosexual men, but that reductions were less substantial among women aged 25 and older.
This is thought to be because women are more likely to achieve viral suppression through the uptake and effective use of HIV treatment, preventing them from transmitting HIV to their male partners, but the reverse is not the same thing.
Gender disparity
The analysis showed that the number of women reaching and maintaining undetectable (non-transmissible) levels of HIV infection was 1.5 to 2 times higher than men of all ages in 2018. The analysis showed shows that if men had achieved the same levels of virus suppression as women, about half of new infections that occurred between 2016 and 2018 could have been avoided.
The team also reconstructed transmission networks based on the virus’s genetic code from thousands of participants, which confirmed that overall the proportion of transmissions from men is increasing and now accounts for 63% of all transmissions in the region, although more women than men are living with HIV.
The team says the disparity could be because men have to travel for work, clinics are closed when they return home, or for other reasons, including social stigma.
Dr Oliver Ratmann, lead author of the study from Imperial’s Department of Mathematics, said: “In this ever-evolving fight against HIV, it is vital that we adapt our strategies, close the gaps in care and ensure that people, regardless of gender, have access to the life-saving benefits of ART.
“It is important to design services so that everyone who wants to use them can and feels empowered to do so. By regularly monitoring the evolving dynamics of the epidemic and fighting for equity in HIV care, we can move closer to the ultimate goal: controlling and one day eliminating HIV transmission. »
Dr. Kate Grabowski, co-author of the study from Johns Hopkins Medical School, added: “The continued success of the President’s Emergency Plan for AIDS Relief (PEPFAR) in reducing infections and saving lives is crucial to ending HIV transmission. “
“As the U.S. Congress currently evaluates funding for PEPFAR, our evidence strongly supports the program’s effectiveness and provides a clear roadmap to ending the pandemic through improved HIV treatment coverage, particularly among men .
Closing the gap in transmission
The team used data from the Rakai Community Cohort Study (RCCS) in southern Uganda, a region where more than 9% of adults are living with HIV, about 20 times more than in the United States. Since 2003, before ART became widely available in Africa, RCCS has recruited nearly 37,000 people, tracking the evolution of HIV infection as new interventions were implemented.
The analysis tracked the changing dynamics of the heterosexual HIV epidemic in 36 communities over a 15-year period using RCCS surveillance data, including records of new infections, HIV genomic data at in-depth sequence, HIV treatment uptake, viral suppression and behavioral information.
Analyzes from previous years showed that the highest number of new HIV cases in southern Uganda were among adolescent girls and young women aged 15 to 24. In the last few years studied in the new study, women aged 25 to 34 became a new focal group, experiencing a slower decline in new infections than other age groups. This is accompanied by a significant difference in the decline in new infections between men and women, with those of boys and men falling much faster.
To estimate the likely impact of bringing men to the same level of viral suppression, the team applied statistical models based on data on transmission dynamics. The resulting projections indicate that closing the viral suppression gap among men could have effectively halved rates of new infections among women and eliminated gender disparities in HIV transmission.
Dr. Joseph Kagaayi, former director of the Rakai Health Sciences program and co-lead author of the study, said: “Our study findings highlight the importance of addressing disparities in ART uptake and withdrawal. viral between men and women. “can not only reduce HIV infections among women, but also work to narrow the gender gap in HIV transmission. Achieving these goals will require concerted efforts, informed policies and strengthened health services.”
More information:
Mélodie Monod et al, Population-level longitudinal HIV epidemiological and genomic surveillance highlights growing gender disparity in HIV transmission in Uganda, Natural microbiology(2023). DOI: 10.1038/s41564-023-01530-8
Provided by Imperial College London
Quote: Engaging heterosexual men more effectively could reduce HIV infections in Uganda (December 8, 2023) retrieved December 8, 2023 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.