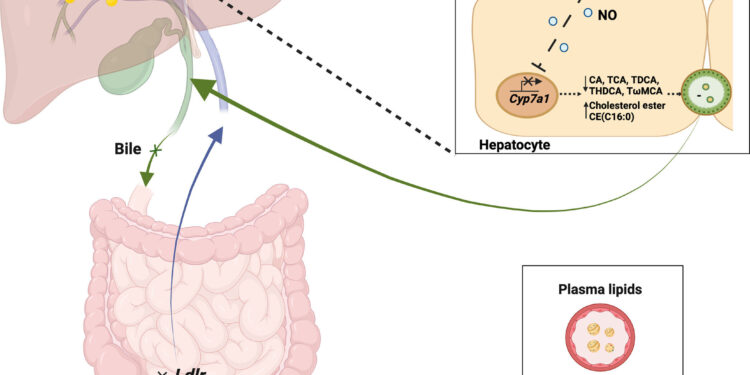
Lipid regulation of parenchymal cells by sensing endothelial force. Credit: Scientific advances (2024). DOI: 10.1126/sciadv.adq3075
A new discovery about how the liver removes cholesterol from the body could lead to more effective treatments for cardiovascular disease, the world’s leading cause of death.
Researchers at the University of Leeds have discovered that the production of bile, which is vital for removing excess cholesterol from the body, is affected by the speed at which blood flows into the liver via the ‘portal’ vein from the ‘intestine.
Previous research has shown that blood flow in the portal vein increases and decreases throughout the day in response to movement, rest, and food consumption. The Leeds team has now identified that bile production increases when blood flow in the portal vein decreases, which occurs following exercise or fasting. Conversely, bile production decreases when blood flow through the portal vein increases, which occurs when people eat and rest.
Low bile production can lead to high levels of cholesterol remaining in the blood, which can contribute to the development of fatty liver disease. If left untreated, this condition can progress to liver inflammation and fibrosis, currently affecting one in three people in the UK.
This breakthrough offers an opportunity for the development of new treatments to combat cardiovascular diseases and prevent the progression of fatty liver disease.
Lead researcher Dr Laeticia Lichtenstein, lecturer in nutrients and metabolism in the School of Food Sciences and Nutrition, said: “This finding that the liver does not have a constant and stable function, but is able to detect changes and adjust its functionality based on the body’s needs, it’s incredible.
“Our results can be used by surgeons and experts in liver and digestive system diseases such as gallstones and liver cirrhosis, in the treatment of their patients, to better understand the origins of these diseases.”
The team’s research, published in Scientific advancesrevealed for the first time that portal vein blood flow is related to blood cholesterol levels.
It shows that a pressure-sensitive protein called PIEZO1 senses blood flow in the vein, triggering a chemical chain reaction that turns cholesterol in the blood into bile acids to be removed from the body.
Liver and heart function
One of the key functions of the liver is to regulate the amount of fat in the blood. So when levels are high, fatty liver can develop. This can damage the liver and lead to more serious illnesses, including cirrhosis, liver failure, and liver cancer.
Cholesterol is a type of fat essential for the body’s normal functioning and is found in every cell in the body. There are two types: the “good” ones which are useful for the functioning of the body and the “bad” ones which can accumulate in the arteries, increasing the risk of heart disease and stroke.
High cholesterol levels may have a genetic basis or be linked to certain medications and health conditions, but they are also associated with lifestyle factors, including a diet high in saturated and trans fats; a lack of physical activity; obesity; smoking and excessive alcohol consumption.
First-line treatments involve adopting a healthier lifestyle, but patients may also be prescribed medications such as statins to reduce so-called “bad” cholesterol. However, some patients may have reduced mobility or suffer from statin-related side effects. Additionally, a better understanding of other factors, such as blood flow and its impact on fat regulation, is needed to improve how drugs work.
Professor David Beech, Principal Investigator from the University of Leeds School of Medicine, said: “Laeticia’s exciting work opens a potentially important new avenue for clinical interventions into the growing global problem of liver dysfunction. »
More information:
Laeticia Lichtenstein et al, Endothelial force detects signals sent to parenchymal cells to regulate biliary and plasma lipids, Scientific advances (2024). DOI: 10.1126/sciadv.adq3075
Provided by the University of Leeds
Quote: Discovery of how the liver removes cholesterol from the body could lead to better treatments for cardiovascular disease (October 18, 2024) retrieved October 18, 2024 from
This document is subject to copyright. Apart from fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.