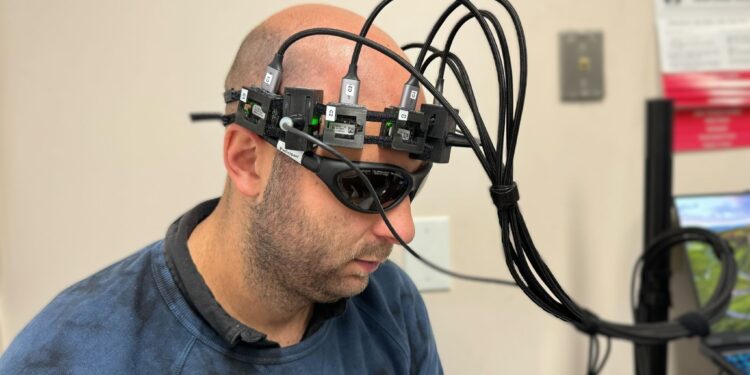
Caltech and USC have developed a new laser helmet that can non-invasively measure blood flow and volume. Simon Mahler, a postdoctoral researcher at Caltech and co-lead author of the paper describing the work, wears the device here. Credit: Caltech
When doctors want to learn more about a patient’s risk of cardiovascular disease, they may order a cardiac stress test. But when it comes to stroke risk, there is no equivalent, scalable, cost-effective test of brain function to help doctors advise patients about their potential risk. A questionnaire that asks patients about contributing risk factors is currently the best tool for estimating this risk.
Now, a team of engineers and scientists from Caltech and the Keck School of Medicine of USC has developed a helmet-based device that can be used to non-invasively assess stroke risk of a patient by monitoring changes in blood flow and volume while a participant holds their breath. The device incorporates a laser system and has shown promising results in differentiating between individuals at low and high risk of stroke.
Stroke affects nearly 800,000 Americans each year and is the leading cause of serious long-term disability in the United States. It is caused by blockage or rupture of an artery in the brain, leading to reduced blood flow. Deprived of oxygen, brain cells die quickly: around 2 million per minute during a stroke.
“With this device, for the first time, we will have a way of knowing whether a person’s risk of having a stroke in the future is significant or not, based on a physiological measure,” explains Simon Mahler, co-senior author of a paper describing the new technique and device, and a postdoctoral researcher in the lab of Changhuei Yang, the Thomas G. Myers Professor of Electrical Engineering, Bioengineering, and Medical Engineering at Caltech and research fellow at the Heritage Medical Research Institute.
“We think this can really revolutionize the way stroke risk is assessed and will eventually help doctors determine whether a patient’s risk is stable or getting worse.”
“Our optical technology for noninvasively measuring blood flow should be useful for a number of applications related to brain diseases,” says Yang, who is also managing director of electrical engineering at Caltech. He noted that this project is part of a larger collaborative effort with Dr. Charles Liu, professor of clinical neurological surgery, surgery, psychiatry, behavioral sciences and biomedical engineering at the Keck School of Medicine in USC, and his team.
The article, titled “Correlating stroke risk with noninvasive cerebrovascular perfusion dynamics using a portable speckle contrast optical spectroscopy laser device,” appears in Express Biomedical Optics.
Speckled Contrast Optical Spectroscopy for Stroke Risk Assessment
In general, blood vessels become stiffer as a person ages, meaning they have a harder time expanding to allow blood to pass through. This means that the person is more prone to strokes.
The Caltech team developed a compact device that shines infrared laser light through the skull and into the brain in a single location, then uses a special nearby camera to collect the light that bounces back after being scattered by circulating blood in the blood vessels.
The approach, called optical speckle contrast spectroscopy (SCOS), measures the decrease in light intensity from where it enters the skull to where the reflected light is collected to determine the volume of blood in the blood vessels of the brain; it also looks at how light scatters and creates spots in the camera’s field of view.
The spots vary in the images depending on the blood flow in the blood vessels. The faster the blood circulates, the faster the spot field changes.
Researchers can use these measurements to calculate a ratio between the flow rate and volume of blood flowing through the vessel to get an idea of that patient’s risk of stroke.
In the new study, researchers from Caltech and the Keck School of Medicine of USC tested the new device on 50 volunteers split between high and low stroke risk. After a minute, participants were asked to hold their breath, which caused blood to rush to the brain. The headset used contrast speckle optical spectroscopy (SCOS) to measure changes in blood flow and volume. Based on these measurements, the device was able to successfully differentiate between low-risk and high-risk participants. Credit: Huang et al., Express Biomedical OpticsSeptember 2024.
The team conducted a study with 50 participants. They used the currently used stroke risk questionnaire, the Cleveland Stroke Risk Calculator, to divide participants into two groups: one at low risk and one at high risk. They then measured each volunteer’s blood flow for three minutes, quantifying the flow and volume of blood reaching the brain. After a minute, they asked the participants to hold their breath.
Holding your breath stresses your brain because it begins to notice that it’s taking in too much carbon dioxide and not enough oxygen. He enters what Mahler calls “panic mode” and begins pumping oxygen from the rest of the body to himself. This significantly increases blood flow to the brain.
Once you stop holding your breath, oxygen levels return to baseline. Although this occurred in people at low or high risk of stroke, researchers found that there were differences between the groups in terms of how blood flowed through the vessels.
The SCOS technique allows researchers to measure how much blood vessels dilate while the subject holds their breath and how quickly blood flows through the vessels in response. “These reactive measurements indicate the stiffness of the vessels,” explains Yang. “Our technology makes it possible for the first time to perform this type of measurement in a non-invasive manner.”
“What we found is clear and striking evidence of a different response in blood flow and blood volume between the two groups,” says Yu Xi Huang, co-senior author of the new paper and a graduate student in Yang’s lab.
In the low-stroke risk group, researchers observed a smaller increase in blood flow during apnea exercise compared to the high-stroke risk group, but a greater increase in volume blood, indicating that more blood is able to flow. circulate in the enlarged blood vessels.
“We can clearly see that the higher risk group has a higher flow-to-volume ratio, where they have faster flow but lower blood volume during apnea,” says Mahler. This is due to the stiffness of the blood vessels and indicates a higher risk of rupture. “If someone came in with an extremely high flow-to-volume ratio, we might suspect that person will have a stroke in the near future.”
A promising future
The team is conducting additional research using the current prototype imaging device on patients at a hospital in Visalia, California, to gather additional data from a larger, more diverse population. The researchers also plan to integrate machine learning into the device’s data collection process and conduct a clinical trial involving monitoring patients over two years to improve the technology.
They hope the device can eventually be widely used, not only for pre-screening for stroke risk, but also to help detect where exactly in the brain a stroke might have already occurred.
More information:
Correlation of stroke risk with non-invasive cerebrovascular perfusion dynamics using a portable speckled contrast optical spectroscopy laser device. Express Biomedical Optics (2024).
Provided by California Institute of Technology
Quote: Device offers first portable and affordable method to differentiate stroke risk based on physiological conditions (September 30, 2024) retrieved September 30, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.