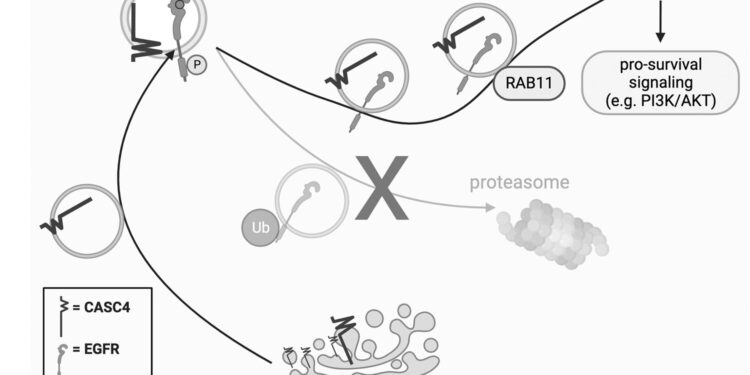
Working model of the CASC4 function. CASC4 drives the recycling of internalized EGFR by promoting its localization in RAB11+ recycling endosomes and suppressing its ubiquitination. Recycling of EGFR to the cell surface allows for continued pro-survival signaling. Created using BioRender. Credit: Cancer gene therapy (2023). DOI: 10.1038/s41417-023-00703-1
A team of researchers at the University of Colorado Anschutz Medical Campus has gained attention for their work to rethink the progression and treatment of ovarian cancer. Equipped with highly advanced technology, they are making progress in making the deadliest cancer of the female reproductive system less deadly.
The American Cancer Society predicts that more than 12,000 women will die from ovarian cancer in the United States this year alone.
“Ovarian cancer progresses with only vague symptoms, leading to delayed diagnosis,” said Lindsay Brubaker, MD, gynecologic oncologist and assistant professor in the division of gynecologic oncology in the Department of Obstetrics and Gynecology at the University of Colorado School of Medicine (SOM).
Brubaker is working closely with ovarian cancer biologist Benjamin Bitler, Ph.D., associate professor in the Division of Reproductive Sciences, to better understand drivers of progression and chemoresistance in ovarian cancer.
“The vast majority of patients who are diagnosed with high-grade serous carcinoma are at an advanced stage, and most cancers will recur,” Brubaker said of the most common subtype, which arises primarily from the fallopian tubes. rather than ovaries. .
In high-grade serous carcinoma, cells found at the end of the fallopian tube in the fimbriae – finger-like projections directly next to the ovaries – break away from the epithelium and travel to different areas of the body, including the ovaries and abdominal cavity. When and how this occurs is still the subject of active research.
In 2019, Brubaker and Bitler took an unbiased genome-wide approach with CRISPR (clustered regularly interspaced short palindromic repeats)/Cas9 gene editing technology and identified critical disease drivers, including several were new and had not previously been associated with ovarian disease. cancer. The results of this genome-wide experiment laid the foundation for future experiments and brought researchers closer to a better understanding of the disease.
Since then, researchers have tracked important genes from the CRISPR study to better understand the mechanisms governing ovarian cancer and develop treatments.
One of the main genes identified was CASC4, but very little was known about this gene. In a new study, published in November in Cancer gene therapyThe Bitler Lab showed that high CASC4 expression is associated with poor clinical outcomes in high-grade serous carcinoma.
Mechanistically, they discovered that CASC4 helps cancer cells evade death, both during disease progression and during chemotherapy treatment. Their work suggests that CASC4 could one day be used as a new biomarker to detect early stages of disease and improve the effectiveness of chemotherapy.
Additionally, researchers used the results of the CRISPR study to develop inhibitors targeting new cancer genes. Last year they published another study, in Expert opinion on therapeutic targets, in which they designed a peptide that blocks CBX2, a protein that promotes ovarian cancer progression and resistance to chemotherapy. The peptide successfully inhibited tumor progression in vitro and in vivo.
Currently, Brubaker and his team are trying to further improve the effectiveness of the peptide, with the goal of using it in future clinical trials.
“All of these projects came out of the original CRISPR paper,” Bitler said. The progress they made “would not have been possible without (Brubaker’s) seminal work,” he said.
“We are very fortunate here at the University of Colorado to have access to an incredible range of expertise and technology,” Brubaker said, attributing much of his team’s success to CU’s collaborative environment Anschutz and to world-class resources on campus, such as the Functional Genomics Shared Resource.
Next step: tackling chemotherapy resistance
According to Brubaker, ovarian cancer is usually treated with a combination of surgery and chemotherapy; However, over time, tumor cells develop resistance to chemotherapy, particularly platinum-based drugs.
“Our goal is to understand what drives chemoresistance in high-grade serous carcinoma and how can we target these pathways and resensitize tumor cells to chemotherapy,” she said.
Brubaker’s team plans to develop new drugs and test existing drugs that could work as a new targeted cancer therapy, she said. Traditional chemotherapy can be very toxic. The hope is to find targeted therapies that will keep the cancer at bay while improving the patient’s quality of life, Brubaker said. Brubaker, Bitler and the Bitler Lab are committed to better understanding high-grade serous carcinoma and identifying new treatment options.
More information:
Jaidev Bapat et al, CASC4/GOLM2 promotes anoikis resistance in high-grade serous carcinoma through EGFR recycling, Cancer gene therapy (2023). DOI: 10.1038/s41417-023-00703-1
Lindsay W. Brubaker et al, New chromobox 2 inhibitory peptide reduces tumor progression, Expert opinion on therapeutic targets (2023). DOI: 10.1080/14728222.2023.2218614
Provided by CU Anschutz Medical Campus
Quote: CRISPR study lays foundation for fight against ovarian cancer (January 30, 2024) retrieved January 30, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.