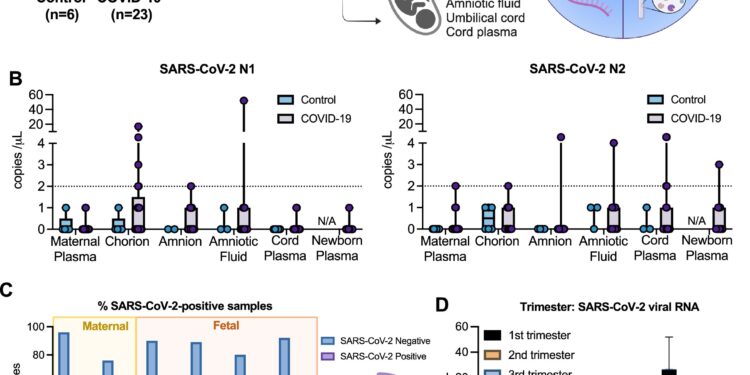
Vertical transmission rates in maternal-fetal biological samples derived from the COVID-19 affected pregnancy cohort. Credit: EMBO magazine (2024). DOI: 10.1038/s44318-024-00260-9
A new study led by the Cleveland Clinic and published in EMBO magazine shows that mild, asymptomatic SARS-CoV-2 infections can trigger immune responses in a pregnant person that can cause severe inflammatory responses in the developing fetus.
The study results also suggest that vertical transmission of the virus from a pregnant person to the fetus is more common than previously estimated and that even without this transmission, a pregnant person’s immunological response to the virus The infection can have an impact on the fetus.
Typically, healthcare providers test a newborn for infection with SARS-CoV-2, the virus that causes COVID-19, using a nasal swab after birth. For this study, Cleveland Clinic researchers collected samples from the placenta and fetal compartment (tissues that surround the fetus while it is still in utero), then analyzed them for the presence of inflammatory markers and the virus. .
They found higher instances of virus in these tissues than could be found in a traditional nasal swab, and even in the absence of full infection, they found that small proteins from the virus had crossed the placenta.
The researchers hope their study will help ensure that pregnant women can quickly and reliably receive the evidence-based medical care needed during new outbreaks and public health crises.
When the COVID-19 pandemic began, obstetrician-gynecologist Ruth Farrell, MD, and colleagues at the Cleveland Clinic and other major medical centers wanted to determine how best to prevent and manage infection in their pregnant patients. Pregnant people have required different medical considerations during the pandemic compared to their non-pregnant counterparts; Dr. Farrell notes that many of the prevention and treatment approaches used in non-pregnant patients either did not have enough data to be used in pregnant patients or were not feasible.
“Early in the pandemic, there were significant delays in determining how best to prevent and treat pregnant patients infected with SARS-CoV-2,” says Dr. Farrell, who is also vice president of research for obstetrics at the Cleveland Clinic. & Institute of Gynecology
“These delays are leading to gaps in our understanding of the COVID pandemic for pregnant people. These gaps also contribute to the disparities that have prevented pregnant people from accessing the best possible treatment as quickly as possible during the pandemic.
Dr. Farrell worked with clinical colleagues at the Northern Ohio Clinical and Translational Science Collaborative (CTSC) to develop methods to examine the impact of SARS-CoV-2 infection on pregnant patients , including researchers from University Hospitals Cleveland and MetroHealth Medical Center.
She then teamed up with Cleveland Clinic maternal-fetal virologists Jolin (Suan Sin) Foo, Ph.D. and Javier (Weiqiang) Chen, Ph.D. of the Infection Biology Program to determine the impact of virus on the immune system of the mother and child.
When the standard COVID-19 test is used to detect the virus in newborns (nasal swabs at birth), they only detect infections in about 2% of children whose mothers tested positive for the virus during pregnancy. pregnancy. However, when Drs. Chen and Foo examined the tissues that surrounded newborns while they were still in utero, including amniotic fluid, chorion and umbilical cord plasma, and detected high levels of virus in more than a quarter ( 26%) of study participants.
The team also found elevated immune and inflammatory responses affecting the pregnancies of approximately 66% of study participants. Dr. Foo had previously shown high levels of fetal inflammation in pregnant women who suffer severe SARS-CoV-2 infections during pregnancy, but few people questioned whether asymptomatic or mild infections had the same effect. But now that they had their answer, the team was faced with even more questions.
“Even though we only saw vertical transmission of the full viral infection in a quarter of cases, we saw strong immune and inflammatory responses in more than two-thirds of cases,” says Dr. Foo. “It was clear that even when fetuses weren’t technically infected, they were still affected by their mother’s viral infection. But we didn’t really know how.”
High levels of inflammation during pregnancy, in COVID and other conditions, can have negative impacts on offspring long after birth. Further research could define how inflammation affects children in the long term.
Dr. Chen noted that the SARS-CoV-2 virus has a protein called ORF8 that physically resembles a human immune protein called immunoglobulin G that crosses the placenta from mother to fetus during development. He wonders if the viral protein could also pass through the placenta’s defenses to cause inflammation in the fetal compartment.
Drs. Foo and Chen, alongside co-first authors Tamiris Azamor, Ph.D. and Débora Familiar-Macedo, Ph.D. (a former and current postdoctoral researcher in Dr. Foo’s lab, respectively), were able to prove that ‘ORF8 made by the virus actually passed through the placenta to the fetus. ORF8 then bound to immune proteins and “activated” a process called the complementary immune response.
At normal levels, the complement system is a good thing during pregnancy and helps the fetus develop properly, says Dr. Familiar-Macedo. At higher levels, the complement system can cause dangerous inflammation in the developing fetus. Laboratory studies have shown that this immune response directly leads to the high levels of inflammation seen in the fetuses of pregnant patients infected with the SARS CoV-2 virus.
“Our results challenge the currently accepted definition of vertical transmission, or what it means to pass an infection from mother to fetus,” says Dr. Chen. “We have shown that it is indeed possible for only a small part of a virus to spread and affect a pregnancy.”
Dr. Foo adds that she hopes her team’s findings will serve as guidelines for healthcare practitioners, researchers and policy makers in their further research into vertical transmission and long-term care.
“We showed that the misconception that uninfected babies born to infected mothers are fine is sometimes just that: a misconception,” she says. “Pregnancy is such a vulnerable nine-month period where any change from the norm can have long-term consequences for the baby. We therefore need to work more closely with these individuals to understand their unique health care needs during public health crises. only way to ensure they receive the care they need.
More information:
Tamiris Azamor et al, SARS-CoV-2 ORF8 transplacental protein binds to complement C1q to trigger fetal inflammation, EMBO magazine (2024). DOI: 10.1038/s44318-024-00260-9
Provided by Cleveland Clinic
Quote: COVID study reveals virus-induced inflammation during pregnancy, redefines vertical transmission (October 16, 2024) retrieved October 16, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.