Credit: Unsplash/CC0 Public Domain
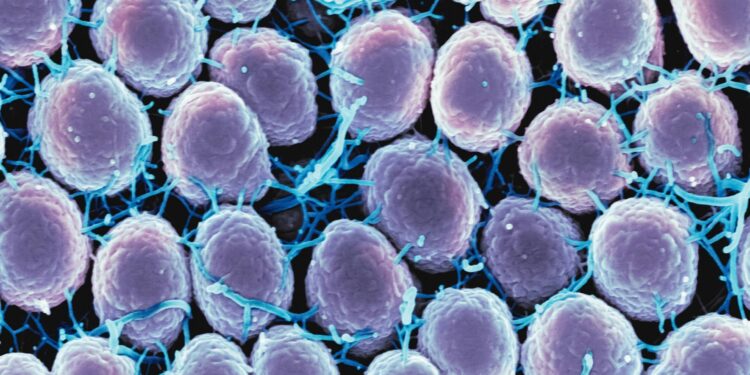
Study of Kenyan sex workers sheds light on immune response to gonorrhea, paving the way for more effective vaccines.
Conducted by scientists from the Universities of Manchester and Oxford in collaboration with the KEMRI/Wellcome Trust Unity in Kenya, the study is published in the journal Nature Communications.
The findings come as recent reports show that gonorrhea, a sexually transmitted disease, is becoming increasingly resistant to antibiotics and may become incurable in the future.
People infected with gonorrhea may experience pain or burning, but if left untreated, they can develop more serious problems, including infertility, systemic infection, and increased risk of HIV/AIDS. Today, there are multidrug-resistant strains of the bacteria Neisseria gonorrheae (Ng), which causes gonorrhea, making many antibiotics ineffective as first-line treatment.
The bacteria have a series of mechanisms to dampen immune responses, meaning there is not enough immunological “memory” to fight off subsequent infections.
Attempts to develop a vaccine against gonorrhea have been largely unsuccessful. However, in 2017, a study showed that vaccination against a related bacterium, Neisseria meningitidis (Nm), resulted in a reduction in the incidence of gonorrhea. Although the efficacy of the Nm vaccine against Ng is limited, it provided an important lead for the development of an effective Ng vaccine.
Working with a marginalised community of sex workers on the Kenyan coast who are at high risk of gonorrhoea, Professor Ed Sanders and his team in Kenya conducted a trial of a Nm vaccine to examine their immune responses. Professor Jeremy Derrick and his team in Manchester then identified the pattern of antibody responses in vaccinated people and compared them to those infected with gonorrhoea.
To decipher the complex antibody responses, the Manchester team built a “microarray” – a library of different components, or antigens, that could react with the antibodies induced by the Nm vaccine. Using this powerful technology, the complex profiles of antibodies against the different components were determined for each vaccine recipient, or each infected individual.
Comparing the profiles revealed a detailed picture of antibody responses to the vaccine, showing how they differ from those following infection.
Professor Chris Tang, project leader at the University of Oxford, said: “This work is an important step towards developing vaccines against Ng, as we have a better idea of the responses generated by partially protective vaccination compared to infection.”
Professor Derrick added: “This study has broad implications for revisiting vaccine design against other bacterial pathogens using these new methods, including those where antimicrobial resistance is a problem. We hope that application of these technologies will enable progress towards vaccines against other pathogens.”
More information:
Stejskal, L., et al. Profiling IgG and IgA antibody responses to vaccination and infection in a population at high risk for gonorrhea. Nature Communications (2024). DOI: 10.1038/s41467-024-51053-x
Provided by the University of Manchester
Quote:Collaborative study brings effective gonorrhea vaccine closer (2024, August 21) retrieved August 21, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.