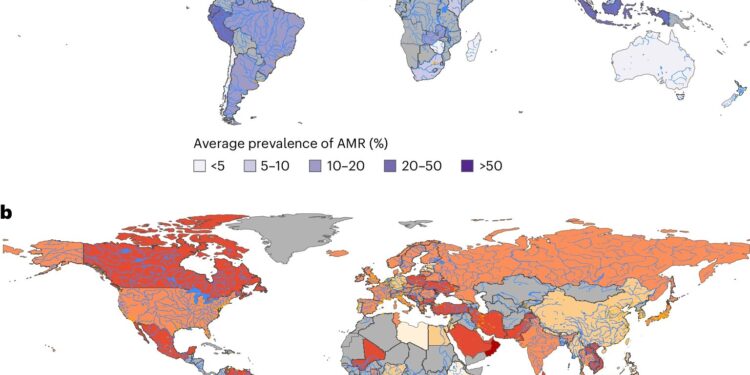
Global distribution and annual changes in RAM. Credit: Nature Medicine (2025). DOI: 10.1038 / S41591-025-03629-3
Current climate change trajectories and non-compliance with sustainable development strategies could contribute to an increase in the global burden on antimicrobial resistance (AMR) by 2050, according to a study published in Nature Medicine. The authors project that the AMR could increase up to 2.4% in the world by 2050, and calls for urgent action to treat wider socio-economic and environmental factors beyond the simple reduction in the use of antibiotics to mitigate the global load of the AMR.
In 2021, bacterial AMR was responsible for around 1.14 million deaths worldwide, affecting low and average income countries disproportionately. This number should increase to nearly 2 million deaths by 2050. Recognizing the severity of the AMR burden, the world leaders of the 79th General Assembly of the United Nations published a declaration which undertakes to reduce the 4.95 million human death bachelor of the AMR by 10% by 2030.
However, a large part of the AMR response focused on an excessive use of antibiotics, and less attention was paid to the context of climate change and socioeconomic conditions.
The researcher Lianping Yang and his colleagues have analyzed 4,502 recordings encompassing 32 million isolates of 6 Key Bacterial Agents resistant to antimicrobial resistant, obtained from 101 countries between 1999 and 2022. Using forecast models, they studied how socio-economic and environmental factors and policies would influence global trends.
Their results suggest that in the worst of the climate change adaptation scenario, in which global temperatures would increase from 4 to 5o C at the end of the century (SSP5–8.5), the AMR could increase by 2.4% by 2050, compared to the low -emission scenario (SSP1–2.6). This varied between 0.9% in high -income countries, and 4.1% and 3.3% in lower countries and low -income countries, respectively.
Yang and his colleagues also found that sustainable development efforts, such as the reduction in health spending, expanding immunization coverage, increasing health investments and guaranteeing universal access to water, health services and hygiene, could reduce the future AMR prevalence by 5.1% compared to the database. This would exceed the effect of reducing antimicrobial consumption, which should reduce the prevalence of the AMR by 2.1%.
The authors recognize that causality cannot be drawn due to the approach to ecological modeling, as well as the limits of the quality of AMR surveillance data sets. In addition, the main models do not take into account certain factors that contribute to RAM, such as education, the use of antimicrobials in food production and animal agriculture practices, due to the unavailability of data.
More information:
Weibin Li et al, the evolution of the climate and socioeconomic factors contribute to global resistance to antimicrobials, Nature Medicine (2025). DOI: 10.1038 / S41591-025-03629-3
Supplied by nature publishing group
Quote: Climate change and lack of sustainable policies can increase the increase in superbugs (2025, April 28) recovered on April 28, 2025 from
This document is subject to copyright. In addition to any fair program for private or research purposes, no part can be reproduced without written authorization. The content is provided only for information purposes.