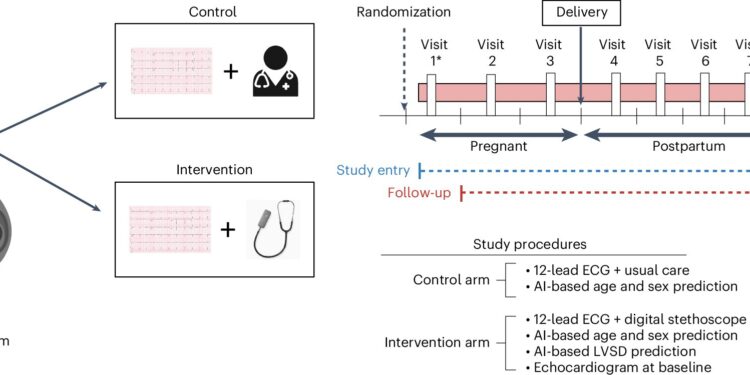
Summary of study design. This figure summarizes the study design, interventions, study visits, and key study procedures. Participants could enter the study at any time during pregnancy or postpartum (up to 12 months). Thus, each participant could have a maximum of seven visits if she entered the study during the first trimester of pregnancy and fewer depending on the timing of study entry. AI-based screening was performed up to seven times during the study period, including during each trimester of pregnancy (first trimester, <14 weeks; second trimester, 14 to <28 weeks; and third trimester, 28 to <42 weeks and postterm) (up to three ECGs), between delivery and 6 weeks, between 6 weeks and 3 months, between 3 and 5 months, and between 5 and 12 months postpartum (up to four ECGs). Only participants in the intervention group underwent a baseline echocardiogram and a simultaneous portable ECG recorded at each time point. AI-based prediction for LVSD using the digital stethoscope was available in real time at the point of care, and 12-lead AI-ECG predictions for LVSD were provided asynchronously, typically within 1 week of ECG acquisition. *Visit 1 may vary for each participant based on the timing of study entry relative to delivery. Credit: Natural medicine (2024). DOI: 10.1038/s41591-024-03243-9
Heart failure in pregnancy is a dangerous and often under-detected condition because common symptoms—shortness of breath, extreme fatigue, and difficulty breathing when lying down—are easily mistaken for typical pregnancy discomforts. Breaking news research presented at the European Society of Cardiology meeting on a Mayo Clinic study showed that a digital stethoscope powered by artificial intelligence (AI) helped doctors identify twice as many cases of heart failure compared with a control group that received standard obstetric care and screening. The full study results are published in Natural medicine.
The trial was conducted in Nigeria, where more women than anywhere else in the world suffer from pregnancy-related heart failure. The results also show that the screening, including the AI-enabled digital stethoscope, was 12 times more likely than traditional screening to flag heart pump weakness when assessed at an ejection fraction threshold of less than 45%, which is the threshold for a specific type of heart failure called peripartum cardiomyopathy.
“Recognizing this type of heart failure early is important for the health and well-being of the mother,” said Dr. Demilade Adedinsewo, a cardiologist at the Mayo Clinic and lead researcher on the study.
“Symptoms of peripartum cardiomyopathy can get progressively worse during pregnancy, or more commonly after delivery, and can be life-threatening if the mother’s heart becomes too weak. Medications can help when the condition is identified, but severe cases may require intensive care, a mechanical heart pump, or sometimes a heart transplant if not controlled with medical treatment.”
The randomized, controlled, open-label clinical trial included nearly 1,200 participants who were screened for heart problems through standard obstetric care or AI-enhanced solutions. Mayo Clinic researchers previously developed a fundamental AI-based 12-lead electrocardiogram (ECG) algorithm to predict a weak heart pump, clinically known as low ejection fraction. A version of this algorithm was further enhanced by Eko Health for its point-of-care digital stethoscope, which is approved by the U.S. Food and Drug Administration (FDA) to detect heart failure with low ejection fraction.
The researchers found that physicians using AI-based screening with the digital stethoscope and 12-lead ECG detected poor heart function with high accuracy. In the study cohort, the digital stethoscope flagged twice as many cases of low ejection fraction <50% and physicians using it were 12 times more likely to identify an ejection fraction <45% compared to usual care.
The AI-based tools were evaluated at three different levels of ejection fraction used in clinical diagnosis. Less than 45% is the threshold for diagnosing peripartum cardiomyopathy. Less than 40% indicates heart failure with reduced ejection fraction and is strong evidence for specific medications to reduce symptoms and risk of death.
An ejection fraction less than 35% signals severely reduced cardiac pump function that often requires more intensive management, including advanced heart failure therapies and an implantable cardioverter-defibrillator if pump function does not recover. Patients in the intervention group each underwent an echocardiogram at study entry to confirm the AI predictions.
“This study provides evidence that we can better detect peripartum cardiomyopathy in women in Nigeria. However, there are still many questions to be answered,” says Dr. Adedinsewo. “Our next steps will be to evaluate the usability and adoption of this tool by Nigerian healthcare providers (including physicians and nurses) and, most importantly, its impact on patient care. Peripartum cardiomyopathy affects approximately 1 in 2,000 women in the United States and up to 1 in 700 African-American women. Evaluating this AI tool in the United States will allow for further testing of its capabilities in diverse populations and healthcare settings.”
More information:
Demilade A. Adedinsewo et al, Artificial intelligence-guided screening of cardiomyopathies in an obstetric population: a pragmatic randomized clinical trial, Natural medicine (2024). DOI: 10.1038/s41591-024-03243-9
Quote: AI Stethoscope Doubles Detection of Heart Failure During Pregnancy (September 3, 2024) Retrieved September 3, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.