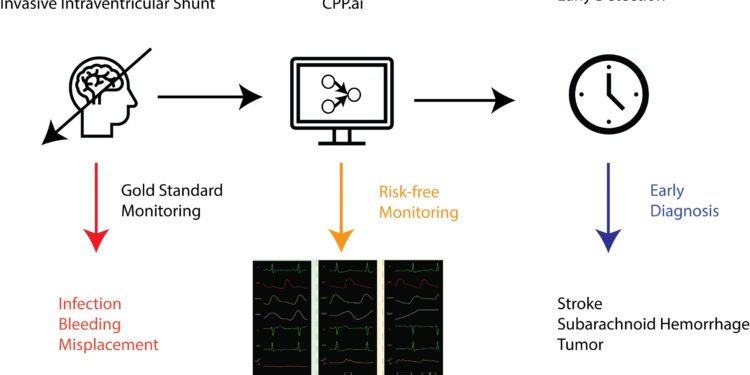
AI-derived intracranial pressure monitors vital information noninvasively, increasing accessibility and reducing risk. In doing so, it could enable healthcare providers to intervene more quickly to save lives. Credit: Faris Gulamali and the lab of Dr. Girish Nadkarni, Ph.D., at Icahn Mount Sinai
Researchers at the Icahn School of Medicine at Mount Sinai have developed a noninvasive technique that could dramatically improve how doctors monitor intracranial hypertension, a condition in which increased pressure in the brain can lead to serious consequences such as stroke and bleeding.
This new approach, based on artificial intelligence (AI), offers a safer and faster alternative to the current skull drilling procedure. Details are presented in Digital medicine npj.
Currently, detecting and monitoring elevated brain pressure requires invasive procedures that puncture the skull. So the research team investigated whether intracranial pressure could be predicted by analyzing noninvasive waveform data, such as electrocardiograms, oxygen saturation levels obtained by pulse oximetry, and waveforms obtained from routine cranial ultrasound scans in intensive care patients.
They then developed an AI model that could generate a representation of cerebral blood pressure. The model was trained using anonymized patient data from patients whose intracranial pressure was measured using invasive methods, such as lumbar catheters or pressure-sensitive probes inserted into the skull. The real-time monitoring tool can quickly detect critical changes, allowing healthcare providers to intervene more quickly and potentially save lives, the researchers say.
“Increased pressure in the brain can lead to a range of serious complications. We created a noninvasive approach – an AI-derived biomarker to detect elevated brain pressure – using data already routinely collected in intensive care units (ICUs),” said first author Faris Gulamali, MD candidate at Icahn School of Medicine at Mount Sinai. “Importantly, our study, the largest to date on intracranial hypertension, is the first to provide external validation of our algorithm and demonstrate a direct link between the biomarker and clinical outcomes, which is required for FDA approval.”
The study, a retrospective analysis, used data from two hospitals in different U.S. cities. The tool performed well in detecting intracranial pressure within seconds. During a patient’s admission, being in the top 25% of intracranial pressure measurements was linked to a 24-fold increase in the risk of subdural hemorrhage and a seven-fold increase in the likelihood of needing a craniectomy (a surgical procedure to relieve pressure on the brain).
The researchers emphasize that the clinical outcome data are correlational, not causal, and that more research is needed to fully establish causality. They then plan to conduct additional validation studies, including those focused on identifying patients with neurological disorders in the intensive care unit. In addition, they hope to apply for breakthrough device status from the FDA, which could bring this lifesaving technology closer to widespread clinical use.
“Our vision is to integrate this tool into intensive care units as a standard part of monitoring critically ill patients. This technology represents a major step forward, potentially transforming the way we manage critically ill patients, reducing the need for risky procedures and enabling faster responses to neurological emergencies,” said senior author Girish Nadkarni, MD, PhD, the Irene and Arthur M. Fishberg Professor of Medicine at Icahn Mount Sinai, director of the Charles Bronfman Institute of Personalized Medicine and system chief, Division of Digital and Data-Driven Medicine.
“Furthermore, our results suggest that it could be a valuable tool not only in neurology, but also in the management of other serious health problems, such as cardiac arrest, glaucoma and acute liver failure.”
“Our team’s development of this AI-based clinical decision support tool could be a significant step forward in improving health outcomes for critically ill patients. If we can validate the use of this tool, we have the potential to improve patient safety by refining the use of invasive intracranial monitoring in patients with the greatest potential for benefit,” said study co-author David L. Reich, MD, president of Mount Sinai Hospital and Mount Sinai Queens, Horace W. Goldsmith Professor of Anesthesiology, and Icahn Professor of Artificial Intelligence and Human Health at Mount Sinai.
“One of our goals at Mount Sinai is to use technology to bring the right team to the right patient at the right time. This tool exemplifies that commitment, providing a tailored solution that has the potential to improve the quality of care for patients at risk of life-threatening brain injuries.”
More information:
Faris Gulamali et al, Derivation, external and clinical validation of a deep learning approach for the detection of intracranial hypertension, Digital medicine npj (2024). DOI: 10.1038/s41746-024-01227-0
Provided by Mount Sinai Hospital
Quote:AI-Based Tool Could Improve Brain Pressure Monitoring in ICU Patients (2024, September 5) retrieved September 5, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.