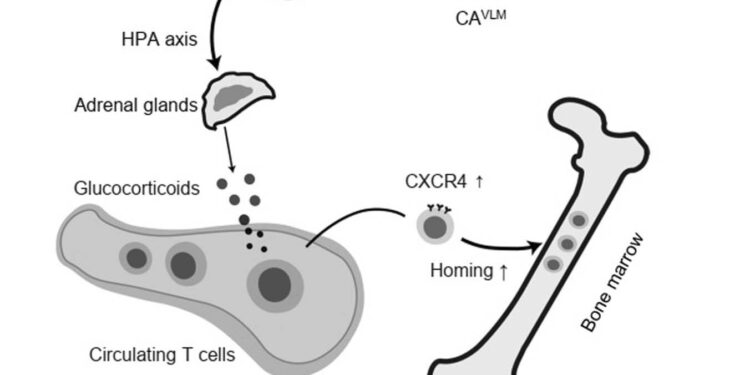
Model of neuronal regulation of the immune system during fasting. Orexigenic ACVLM neurons are activated during fasting, the activation of which stimulates the release of glucocorticoids via the ACVLM→CRHPVN neural circuit targeting the adrenal glands, thereby driving T cells to traffic to the bone marrow in a CXCR4CXCL12 axis-dependent manner and suppressing autoimmune diseases. Credit: Natural neuroscience (2024). DOI: 10.1038/s41593-023-01543-w
Fasting, that is, the voluntary abstaining from eating and sometimes drinking for a specific period of time, is becoming more and more common, as some studies have shown that it can strengthen the immune system and help prevent development of certain diseases. There are now several smartphone apps where people can record their intermittent fasting periods and learn more about the potential benefits of fasting.
Researchers from the University of Science and Technology of China recently conducted a study in mice aimed at better understanding the neural processes underlying the reported effects of fasting on the immune system. Their findings, published in Natural neurosciencesuggest that fasting may specifically promote neuronal control of inflammation and influence the distribution of T cells, a class of white blood cells that help fight germs and protect the body from disease.
“Food fasting significantly influences the distribution and function of immune cells and exerts potent immunosuppressive effects,” Liang Wang, Mingxiu Cheng and colleagues wrote in their paper. “However, the mechanisms by which fasting regulates immunity remain obscure. We report that ventrolateral medulla (VLM) catecholaminergic (CA) neurons are activated during fasting in mice, and we demonstrate that the activity of these CA neurons impact the distribution of T cells and the development of autoimmune diseases in an experimental model of autoimmune encephalomyelitis (EAE).
In their study, Wang, Cheng, and colleagues set out to test a key hypothesis that catecholaminergic (CA) neurons in a region of the brain known as the ventrolateral medulla (VLM), also known as CAVLM Neurons play a role in changes in the mammalian immune system induced by fasting. It has already been shown that these neurons are involved in the responses provoked in the body following nutritional stress, while also influencing inflammation.
CAVLM orexigenic neurons are necessary and sufficient for fasting-mediated T cell redistribution. a, Experimental strategy to identify fasting-activated neurons in the VLM using a FosTRAP assay in Fos2A-iCerER×Ai14 mice. b, Representative images show that fasting caused the expression of tdTomato (red) in TH+ neurons (green) in the VLM. Mice fed ad libitum were used as controls. Arrows indicate double-labeled neurons. c, number of TH+ tdTomato+ double-labeled neurons in the VLM (P = 0.0018). d–g, Impacts of CAVLM neuronal ablation on fasting-mediated T cell redistribution. d, Experimental design to study fasting-mediated T cell redistribution in neuronally ablated CAVLM mice and control mice. After 24 hours of fasting (ZT6–ZT6), mice were killed and tissue samples were collected for further analysis by flow cytometry. e, f, Representative images (e) and group data (f) show selective ablation of CAVLM neurons confirmed by TH immunostaining (green). Scale bars, 200 μm. g, Absolute number of T lymphocytes in blood, BM, spleen, and LNs of neuronally ablated CAVLM mice and control mice. Control mice underwent sham surgery (Ad ctrl n = 6, fasted ctrl n = 8, Ad ablation n = 6, fasted ablation n = 18 biologically independent samples). h–k, Chemogenetic activation of CAVLM neurons redistributes T cells. h, Experimental design. CNO was injected approximately 2 hours after the onset of the light phase (ZT2) and tissue samples were collected at different times after CNO injection. i, Representative image showing selective expression of hM3Dq (red) in CAVLM neurons. j, Activation of CAVLM neurons significantly increased food consumption. k, absolute number of T lymphocytes in blood, spleen, BM and LN 4, 8, 12 and 24 h after CNO injections. n = 7 or 8 mice for each time point (mCherry: 4 hn = 8; 8, 12 and 24 hn = 7 and hM3Dq: 4 and 12 hn = 7; 8 and 24 hn = 8). Credit: Wang et al. (Natural neuroscience2024).
To test this hypothesis, they first examined the activity of these neurons in mice fed regularly and in mice not fed for 24 hours. Additionally, they then selectively ablated and activated these neurons, to observe how their intervention influenced other neuronal mechanisms, as well as the development of autoimmune diseases, in mice.
“CA removalVLM “Neurons largely reversed fasting-mediated T cell redistribution,” Wang, Cheng, and colleagues wrote. “Activation of these neurons led T cells to traffic to the bone marrow in a CXCR4/CXCL12 axis-dependent manner, which may be mediated by a neuronal circuit that stimulates corticosterone secretion. Similar to the Fasting, continuous activation of VLM CA neurons suppressed T cell activation, proliferation, differentiation, and cytokine production in autoimmune mouse models and significantly attenuated disease symptoms.
The results gathered by this team provide valuable new insights into the neural mechanisms that may underlie some of the previously observed benefits of intermittent fasting. More specifically, the team identified a neuronal mechanism that could underlie the regulation of immune cells by fasting.
The neural mechanism they discovered linked to CA activityVLM cells, appears to control the distribution of T lymphocytes, which we already know are linked to inflammation.
This recent work may pave the way for additional studies focusing on the newly identified neural mechanism, which could collectively contribute to the development of fasting-related therapeutic interventions to prevent and treat autoimmune diseases.
More information:
Liang Wang et al, Ventrolateral medulla neurons activated by fasting regulate T cell localization and suppress autoimmune diseases in mice, Natural neuroscience (2024). DOI: 10.1038/s41593-023-01543-w
© 2024 Science X Network
Quote: A neural mechanism that could underlie fasting-mediated immune regulation (February 5, 2024) retrieved February 6, 2024 from
This document is subject to copyright. Apart from fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.