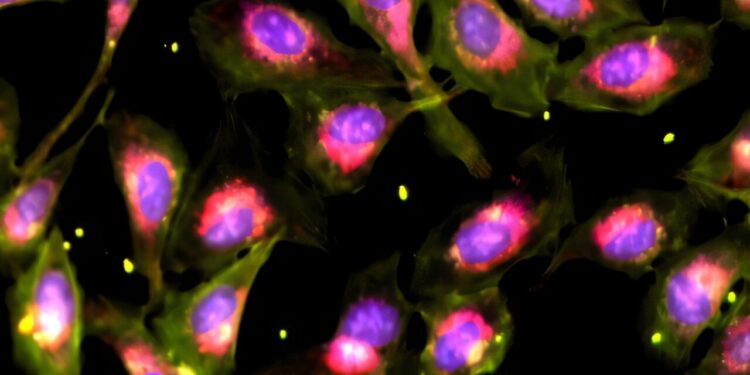
Cell Painting is a test for capturing the characteristics of cell morphology, seen here on the U2OS cell line. Credit: Shalek Lab / Massachusetts Institute of Technology
Some of the most widely used drugs today, including penicillin, were discovered through a process called phenotypic screening. Using this method, scientists essentially use drugs to solve a problem (for example, when trying to stop bacterial growth or repair a cellular defect) and then observe what happens next, without necessarily knowing beforehand how the medicine works.
Perhaps surprisingly, historical data shows that this approach is more effective in producing approved drugs than research that focuses more narrowly on specific molecular targets.
But many scientists believe that the real key to success is defining the problem well. Some microbial infections or genetic disorders caused by single mutations are much simpler to prototype than complex diseases like cancer. These require complex biological models that are much more difficult to create or acquire. This results in a bottleneck in the number of drugs that can be tested, and therefore in the utility of phenotypic screening.
Now, a team of scientists led by MIT’s Shalek Lab has developed a promising new way to solve the difficulty of applying phenotyping screening at scale. Their method allows researchers to apply multiple drugs to a biological problem simultaneously, then work backwards by computer to determine the individual effects of each.
For example, when the team applied this method to models of pancreatic cancer and human immune cells, they were able to uncover surprising new biological insights, while minimizing costs and sample requirements by several times, thereby solving some scientific research problems. .
Zev Gartner, professor of pharmaceutical chemistry at the University of California, San Francisco, says this new method has great potential. “I think if you’re looking at a strong phenotype, that’s going to be a very powerful approach,” Gartner says.
The research was published October 8 in Natural biotechnology. It was led by Ivy Liu, Walaa Kattan, Benjamin Mead, Conner Kummerlowe and Alex K. Shalek, director of the Institute for Engineering and Medical Sciences (IMES) and the Health Innovation Hub at MIT, as well as Professor J.W. Kieckhefer. at IMES and the Department of Chemistry.
A “crazy” way to scale
Technological advances over the past decade have revolutionized our understanding of the internal life of individual cells, paving the way for richer phenotypic screens. However, many challenges remain.
On the one hand, biologically representative models such as organoids and primary tissues are only available in limited quantities. The most informative tests, like single-cell RNA sequencing, are also expensive, time-consuming, and laborious.
That’s why the team decided to test the “bold, maybe even crazy idea” of mixing everything, says Liu, a Ph.D. student in MIT’s Computational and Systems Biology program. In other words, they chose to combine many disruptions – things like drugs, chemical molecules or biological compounds made by cells – into a single preparation, then try to decipher their individual effects by following.
They began testing their workflow by creating different combinations of 316 drugs approved by the U.S. Food and Drug Administration.
“It’s a high bar: basically, it’s a worst-case scenario,” Liu says. “As each drug is known to have a potent effect, the signals might have been impossible to disentangle.”
These random combinations ranged from three to 80 drugs per pool, each applied to cells grown in the laboratory. The team then attempted to understand the effects of each drug using a linear computer model.
It was a success. Compared to traditional testing for each individual drug, the new method yielded comparable results, successfully identifying the most potent drugs and their respective effects in each pool, for a fraction of the cost, samples and effort.
Put it into practice
To test the method’s applicability to address real-world health challenges, the team then addressed two problems previously unimaginable with phenotypic screening techniques of the past.
The first test focused on pancreatic ductal adenocarcinoma (PDAC), one of the deadliest types of cancer. In PDAC, many types of signals originate from surrounding cells in the tumor environment. These signals can influence how the tumor progresses and responds to treatments. The team therefore wanted to identify the most important ones.
Using their new method to group different signals in parallel, they found several surprise candidates.
“We could never have predicted some of our successes,” says Shalek. These included two previously overlooked cytokines that could actually predict survival outcomes of PDAC patients in public cancer datasets.
The second test examined the effects of 90 drugs on adjusting the functioning of the immune system. These drugs were applied to fresh human blood cells, which contain a complex mixture of different types of immune cells. Using their new method and single-cell RNA sequencing, the team was able to not only test a large library of drugs, but also separate the effects of drugs for each cell type. This allowed the team to understand how each drug might work in a more complex tissue, and then select the best one for the job at hand.
“We might say there’s a defect in a T cell, so we’re going to add this drug, but we never think about what does this drug do to all the other cells in the tissue?” Shalek said. “We now have a way to bring this information together so we can begin to select drugs to maximize targeted effects and minimize side effects.”
Together, these experiments also showed Shalek the need to create better tools and data sets to create hypotheses about potential treatments.
“The complexity and lack of predictability of responses we observed indicates to me that we are probably not finding the appropriate or most effective medications in many cases,” says Shalek.
Reduce barriers and improve lives
Although the current compression technique can identify the disturbances with the largest effects, it is still not able to perfectly resolve the effects of each of them. Therefore, the team recommends that it act as a complement to support additional screening: “Traditional tests that look at the best results should follow,” Liu says.
But it’s important to note that the new compression framework significantly reduces the number of input samples, costs, and labor required to run a screen. With fewer hurdles at play, this marks an exciting advance in understanding complex responses in different cells and building new models for precision medicine.
Shalek says: “This really is an incredible approach that opens the door to the kinds of things we can do to find the right targets, or the right drugs, to use to improve patients’ lives. »
More information:
Nuo Liu et al, Scalable and compressed phenotypic screening using pooled disturbances, Natural biotechnology (2024). DOI: 10.1038/s41587-024-02403-z
Provided by the Massachusetts Institute of Technology
This story is republished courtesy of MIT News (web.mit.edu/newsoffice/), a popular site that covers news in MIT research, innovation and education.
Quote: A more efficient phenotypic screening method can test multiple drugs simultaneously (October 17, 2024) retrieved October 17, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.