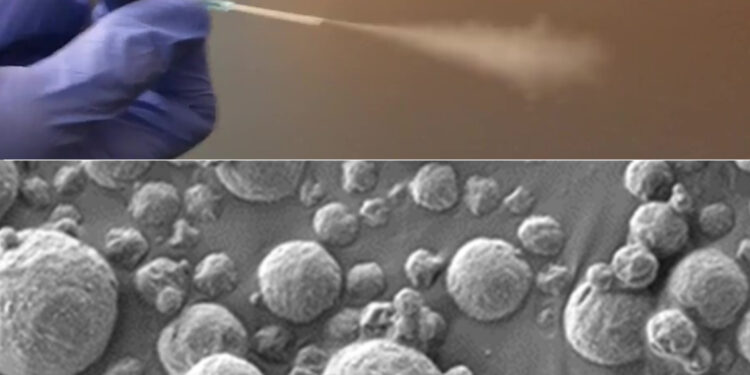
MIT engineers have designed diagnostic particles that can be aerosolized and inhaled. At bottom is a scanning electron micrograph of nanosensor-coated particles that interact with cancer-associated proteins in the lungs. Credit: MIT researchers
Thanks to new technology developed at MIT, diagnosing lung cancer could become as simple as inhaling nanoparticle sensors and then taking a urine test revealing whether a tumor is present.
The new diagnosis is based on nanosensors that can be delivered by an inhaler or nebulizer. If the sensors encounter cancer-related proteins in the lungs, they produce a signal that accumulates in the urine, where it can be detected using a simple paper test strip.
This approach could potentially replace or complement the current gold standard for diagnosing lung cancer, low-dose computed tomography (CT). According to the researchers, this could have a particularly significant impact in low- and middle-income countries that lack widespread access to CT scanners.
“Across the world, cancer will become increasingly prevalent in low- and middle-income countries. The epidemiology of lung cancer globally is that it is caused by pollution and smoking. technology could have a big impact,” says Sangeeta Bhatia, the John and Dorothy Wilson Professor of Health Sciences and Technology and of Electrical and Computer Engineering at MIT, and a member of the Koch Institute for Integrative Cancer Research and from the Institute for Medical. Engineering and science.
Bhatia is the lead author of the article, which appears in Scientists progress. Qian Zhong, a research scientist at MIT, and Edward Tan, a former MIT postdoctoral fellow, are the lead authors of the study.
Inhalable particles
To help diagnose lung cancer as early as possible, the U.S. Preventive Services Task Force recommends that heavy smokers over the age of 50 have an annual CT scan. However, not everyone in this target group receives these scans, and the high false positive rate of the scans can lead to unnecessary and invasive testing.
Bhatia has spent the last decade developing nanosensors for diagnosing cancer and other diseases. In this study, she and her colleagues explored the possibility of using them as a more accessible alternative to CT lung cancer screening.
These sensors are made of polymer nanoparticles coated with a reporter, such as a DNA barcode, that is cleaved from the particle when the sensor encounters enzymes called proteases, which are often overactive in tumors. These reporters eventually accumulate in the urine and are excreted from the body.
Previous versions of the sensors, which targeted other cancer sites such as the liver and ovaries, were designed to be administered intravenously. For lung cancer diagnosis, researchers wanted to create a version that could be inhaled, which could make it easier to deploy in low-resource settings.
“When we developed this technology, our goal was to provide a method that could detect cancer with high specificity and sensitivity, and also lower the threshold for accessibility, so that we could hopefully improve the resource disparity and inequity in early detection of lung cancer,” Zhong said.
To achieve this, the researchers created two formulations of their particles: a solution that can be aerosolized and administered with a nebulizer, and a dry powder that can be administered using an inhaler.
Once the particles reach the lungs, they are absorbed into the tissues, where they encounter any proteases present. Human cells can express hundreds of different proteases, and some of them are overactive in tumors, where they help cancer cells escape from their original location by cutting off extracellular matrix proteins.
These cancer proteases cleave the DNA barcodes from the sensors, allowing the barcodes to circulate in the bloodstream until they are excreted in the urine.
In earlier versions of this technology, researchers used mass spectrometry to analyze the urine sample and detect DNA barcodes. However, mass spectrometry requires equipment that might not be available in low-resource areas. For this version, the researchers therefore created a lateral flow test, which allows barcodes to be detected using a paper test strip.
The researchers designed the strip to detect up to four different DNA barcodes, each indicating the presence of a different protease. No pretreatment or processing of the urine sample is required and results can be read approximately 20 minutes after obtaining the sample.
“We were really pushing this test to be available at the point of care in a low-resource environment, so the idea was to not do any sample processing, not to do any amplification, just to be able to put the sample directly on the paper. and read it in 20 minutes,” says Bhatia.
Accurate diagnosis
The researchers tested their diagnostic system on mice genetically engineered to develop lung tumors similar to those seen in humans. The sensors were administered 7.5 weeks after the tumors began to form, a time point that would likely correlate with stage 1 or 2 cancer in humans.
In their first set of experiments on mice, the researchers measured the levels of 20 different sensors designed to detect different proteases. Using a machine learning algorithm to analyze these results, the researchers identified a combination of just four sensors that should give accurate diagnostic results. They then tested this combination in a mouse model and found that it could accurately detect lung tumors at an early stage.
For use in humans, more sensors may be needed to make an accurate diagnosis, but this could be achieved using multiple paper strips, each of which detects four different DNA barcodes, the researchers say.
The researchers now plan to analyze human biopsy samples to see if the sensor panels they are using would also work to detect human cancers. In the longer term, they hope to carry out clinical trials on human patients. A company called Sunbird Bio has already conducted Phase I trials of a similar sensor developed by Bhatia’s lab, intended to diagnose liver cancer and a form of hepatitis known as nonalcoholic steatohepatitis (NASH).
In areas of the world where access to CT scanning is limited, this technology could offer a dramatic improvement in lung cancer screening, especially since results can be obtained during a single visit.
“The idea would be that you come in and then get an answer as to whether you need a follow-up test or not, and we could bring patients with early lesions into the system so they can benefit curative surgery or life-saving medications,” Bhatia said.
More information:
Qian Zhong et al, Point-of-care inhalable urinary diagnostic platform, Scientists progress (2024). DOI: 10.1126/sciadv.adj9591. www.science.org/doi/10.1126/sciadv.adj9591
Provided by the Massachusetts Institute of Technology
This story is republished courtesy of MIT News (web.mit.edu/newsoffice/), a popular site that covers news about MIT research, innovation and education.
Quote: Inhalable sensors could enable early detection of lung cancer (January 5, 2024) retrieved January 6, 2024 from
This document is subject to copyright. Apart from fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.