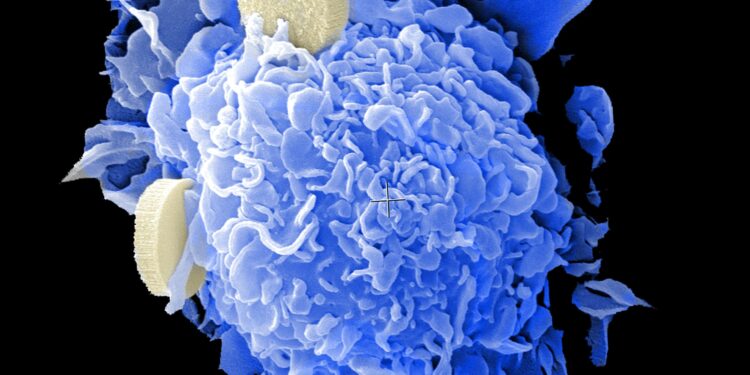
Credit: Unsplash/CC0 Public domain
All cancer mutations that cause drug resistance fall into one of four categories. New research has detailed each type, helping to discover targets for drug development and identify potentially effective second-line therapies.
In a new large-scale study, researchers from the Wellcome Sanger Institute, EMBL European Bioinformatics Institute (EMBL-EBI), Open Targets and collaborators used CRISPR gene editing to map the Genetic landscape of drug resistance in cancers, focusing on colon, lung. and Ewing’s sarcoma. The team explains the impact of known mutations on drug resistance and highlights new changes in DNA that could be explored further.
The research, published in Natural geneticsstudied the effect of mutations on sensitivity to 10 cancer drugs, also identifying possible effective second-line treatments based on a person’s genetic makeup.
By understanding the mechanisms by which cancers become resistant to treatment, researchers can identify new targets for personalized therapies, help treat patients based on the genetic makeup of their cancer, offer second-line treatment options to those who do not currently have one and contribute to the development of research. next-generation anticancer drugs that could prevent the emergence of drug resistance.
One of the major challenges in cancer treatment is drug resistance. Mutations in cancer cells mean that over time they become less responsive to therapies. Once the cancer has become resistant to initial treatment, subsequent therapies are called second-line therapies and the options available for these may be limited. Understanding which molecular changes drive resistance and what can be done to address them can help uncover new options and illuminate clinical pathways for specific mutations.
However, current methods for identifying drug resistance mutations require collecting multiple patient samples over a long period of time, making this process time-consuming and difficult.
To gather large-scale information about cancer mutations, the team from the Wellcome Sanger Institute, EMBL-EBI, Open Targets and collaborators used cutting-edge CRISPR gene editing and single-cell genomics to study the impact of several drugs on human cancer cells. organoid cell lines and models.
By combining these techniques, the researchers were able to create a map showing drug resistance in different cancers, focusing on colon, lung, and Ewing’s sarcoma. The map learns more about the mechanisms of drug resistance, highlights DNA changes that may be potential biomarkers for treatment, and identifies promising combinations or second-line therapies.
The team found that cancer mutations fall into four different categories based on the impact of the change in the DNA. Drug resistance mutations, also called canonical drug resistance mutations, are genetic changes in the cancer cell that make the drug less effective. For example, changes that cause the drug to no longer bind to its target in the cancer cell.
Mutations linked to drug addiction lead some cancer cells to use the drug to help them grow, instead of destroying them. This research supports the use of drug holidays in substance abuse mutations, which are periods without treatment. This could help destroy cancer cells with this type of mutation, because these cells are now dependent on treatment.
Driver mutations are gain-of-function genetic changes that allow cancer cells to use a different signaling pathway to grow, thereby avoiding the pathway that the drug may have blocked.
Finally, drug-sensitizing variants are genetic mutations that make cancer more sensitive to certain treatments and could mean that patients with these genetic changes in their tumor would benefit from particular drugs.
Research has focused on colon cancer, lung cancer and Ewing’s sarcoma cell lines because they are all prone to the development of resistance and have limited second-line treatments. The team used 10 cancer drugs currently prescribed or in clinical trials to help determine whether any of them could be repurposed or used in combination to combat resistance, thereby reducing the time needed to bring the potential treatments in the clinic.
Better understanding the four different types of DNA changes can help inform clinical decisions, explain why treatments don’t work, support the idea of stopping treatment in some patients, and help develop new treatments. This knowledge also helps accelerate pharmaceutical companies’ research into next-generation cancer inhibitors that could better prevent drug resistance.
Dr Matthew Coelho, first author from the Wellcome Sanger Institute and Open Targets, said: “Cancer cells developing resistance to treatments is a huge problem, and having a rapid way to identify these mutations in patients and Understanding how to combat them is essential to achieving this. treat cancer. Our study details how the mutations fall into four different groups, which may require different treatment plans. For example, in cases of drug-related mutations, it may be helpful to take a break from treatment. Using cutting-edge genetic techniques, we began. to build a rapid, large-scale way to understand drug resistance and, hopefully, find new targets for second-line treatments. »
Dr Magdalena Strauss, study author previously at the EMBL European Bioinformatics Institute (EMBL-EBI) and now at the University of Exeter, added: “By combining CRISPR gene editing of state-of-the-art and single-cell techniques with statistical machine learning, we were able to obtain a detailed picture of the specific mechanisms by which each of the individual mutations we studied influences drug response.
“The functional framework we have built allows researchers to begin to comprehensively map the common DNA changes observed during cancer treatment, thereby adding to our collective knowledge. It also highlights mutations that could be used as biomarkers, highlighting cancer cells that are more sensitive to certain treatments, which could help inform future clinical trials.
Dr. Mathew Garnett, lead author from the Wellcome Sanger Institute and Open Targets, noted: “Prior to this study, it was difficult to obtain a large-scale understanding of why and how drug resistance develops in cancer. . This research brings us one step closer to being able to tailor combinations or second-line therapies to a person’s genetic makeup, to try to ensure that treatments are as effective and personalized as possible.
“In addition, we believe that our new systematic approach will be important for understanding the genetic mechanisms of resistance to new drugs in the future. This could help even before resistance emerges in the clinic, and this early information will improve the development of cancer treatments.”
More information:
Core editing screens define the genetic landscape of anticancer drug resistance mechanisms, Natural genetics (2024). DOI: 10.1038/s41588-024-01948-8
Provided by the Wellcome Trust Sanger Institute
Quote: Genetic mapping study reveals four main categories of cancer drug resistance mutations (October 18, 2024) retrieved October 18, 2024 from
This document is subject to copyright. Apart from fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.