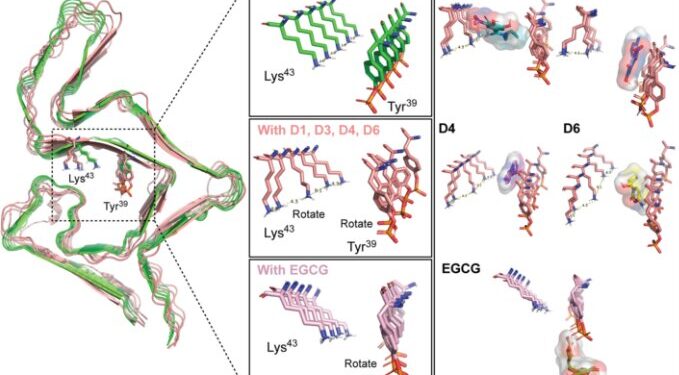
The drug working 3D computational model illustrating the binding interactions between α-SYN aggregates and candidate drugs (D1, D3, D4, and D6) and EGCG at residues Tyr39 and Lys43. Credit: Scientific advances (2024). DOI: 10.1126/sciadv.adk3700
Lewy body dementia (LBD) is a progressive neurodegenerative disease that shares traits with Parkinson’s disease and Alzheimer’s disease, but can be more difficult to diagnose. Symptoms may include hallucinations, movement disorders, cognitive problems, sleep problems and depression.
To better understand how the disease develops, Mayo Clinic scientists created mini brain models on a plate that closely match key features seen in the brains of patients with Lewy body dementia. Mini-brains, also known as cerebral organoids, are clusters of lab-grown cells that mimic the structure of the human brain.
The team also identified four potential drug compounds that may offer promising approaches to treating the disease. Their findings are published in Scientific advances.
There is no cure for LBD, and scientists say there are few accurate preclinical models available to study it. A hallmark of the disease is a protein called alpha-synuclein, encoded by the SNCA gene. This protein is found in nerve cells in the brain and can build up into masses called Lewy bodies, which can contribute to symptoms of dementia.
To better understand the pathology of the disease, a Mayo Clinic research team led by neuroscientist and lead author Na Zhao, MD, Ph.D., developed preclinical mini-brain models using patient stem cells. LBDs that had extra copies of the SNCA gene. , which may have caused their condition. The patients donated their skin cells after diagnosis while they were still alive. Scientists then converted the skin cells into stem cells and used them for research.
Using advanced genomic techniques such as single-cell RNA sequencing, which examines genetic material in individual cells, the researchers showed that their mini-brain models reflected changes seen in the human brains of patients with LBD who had donated their brains to the Mayo Clinic brain bank. , which makes these models valuable tools for studying the development of the disease.
The researchers used their new model system to screen nearly 1,300 drugs approved by the Food and Drug Administration, identifying four candidates that could help prevent the buildup of alpha-synuclein in neurons.
“This study suggests that these mini-brain models can effectively mimic disease development, providing a potential platform for testing individualized treatments for patients,” says Dr. Zhao. “The four identified drug candidates, which have the potential to inhibit alpha-synuclein and restore energy production in neurons derived from patients with LBD, could be further refined or modified to develop new treatments for LBD. LBD and associated dementias in the future.”
The researchers say additional studies could introduce additional cell types to better mimic the complexity of the human brain. Researchers could then use these improved models to study disease mechanisms in more detail, for example by exploring how high-risk genes influence the development of LBD.
More information:
Yunjung Jin et al, Modeling Lewy body disease with SNCA iPSC triplication-derived cortical organoids and identifying therapeutic drugs, Scientific advances (2024). DOI: 10.1126/sciadv.adk3700
Tribune 2024 Content Agency, LLC.
Quote: Researchers create ‘mini-brains’ to model Lewy body dementia and identify treatments (October 14, 2024) retrieved October 14, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.