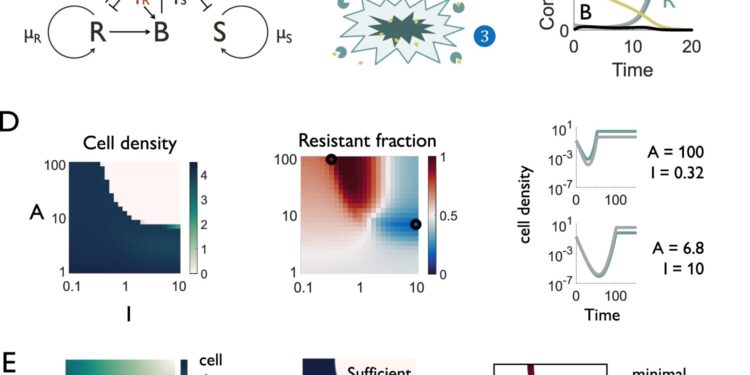
Dynamics of mixed production of good beta-lactamases in a heterogeneous population. Credit: Natural communications (2024). DOI: 10.1038/s41467-024-52711-w
As strains of pathogens resistant to first-line antibiotics become more common worldwide, clinicians are increasingly turning to combination therapies that degrade this resistance as a first treatment option.
Antibiotic-resistant pathogens would therefore be expected to evolve to adapt to this approach. However, previous studies have reached conflicting conclusions about whether this is likely to be the case.
In a study published in Natural communicationsResearchers at Duke University have discovered the mechanism behind these discrepancies: the level of “selfishness” of the bacteria. This information provides guidance to clinicians on how best to tailor these combination treatments to different pathogens, minimize resistance selection, and formulate new antibiotic resistance inhibitors.
“Recent studies have shown a two-fold increase in the prevalence of antibiotic-resistant pathogens in the southern United States over just a five-year period,” said Lingchong You, the James L. Meriam Distinguished Professor of Biomedical Engineering. at Duke. “But this is just the tip of the iceberg. This is a global problem. As doctors increasingly turn to combination treatments, we need to understand how to best implement them to minimize resistor selection.”
The most widely used class of antibiotics worldwide, which includes common drugs like penicillin, are beta-lactam antibiotics. This is also the class of antibiotics to which bacteria are most likely to have developed resistance.
Rather than mutating to avoid antibiotics, bacteria become resistant to beta-lactams by creating an enzyme that breaks down the drug. To combat this resistance, researchers are creating pharmaceuticals that attack and inhibit the enzyme. Used in combination, these inhibitors can restore the effectiveness of beta-lactam antibiotics.
However, previous studies have found discrepancies in how resistant infections respond to these treatments. In some experiments, surviving antibiotic-resistant cells became enriched, increasing their ability to adapt to combination treatments. But in other experiments, the energy cost of creating the antibiotic-degrading enzyme depleted the population of resistant cells, allowing other cells to benefit from their hard work and thrive.
“These seemingly contradictory observations are what motivated our study,” You said. “And the take-home message is very simple: Based on their genetic characteristics, if bacteria are truly selfish with their resistance enzymes, then they will thrive after treatment. But if they are programmed to share their resistance as a public good , then cells that are otherwise sensitive to antibiotics will benefit more.
The enzymes that break down beta-lactam antibiotics are produced and anchored in the outer membrane of a bacteria. This makes them primarily beneficial to the bacteria that produce the enzyme. But as these resistant bacteria break down the drugs around them, they also help protect the population at large. Enzymes can also be released into the environment when resistant bacteria die or because the anchors holding them to the cell are too weak.
These are all natural variables that can either make resistance a private good or a public good, you said. More selfish bacteria are better at latching on to these enzymes, while less selfish strains are not.
To demonstrate how this difference might affect combination therapies, You and his lab created artificial strains that were either very selfish or very generous with their resistance enzymes. Using high-throughput robotic cultivation technology, the lab showed that selfish strains thrived after the combination therapy, while generous strains produced much worse results.
You say these results have two important clinical implications. When using beta-lactam resistance inhibitors, doctors should consider the specific strain being treated. The ability to penetrate bacteria membranes allows selfish bacteria to be better killed, effectively suppressing their selfish traits and minimizing the chances of them developing further resistance. Researchers should look to create inhibitors and other adjuvants that can help these inhibitors be taken up by bacteria.
“Beta-lactam antibiotics and beta-lactam resistance inhibitors are made in standard formulations and cannot be modified, but there are options to choose different formulations together, and this work could help optimize those choices.” , You said. “If we create a database that quantifies how different strains respond to these combinations, it could profoundly improve the quality of treatment.”
More information:
Helena R. Ma et al, The private benefit of β-lactamase dictates the selection dynamics of combined antibiotic treatment, Natural communications (2024). DOI: 10.1038/s41467-024-52711-w
Provided by Duke University
Quote: Targeting “selfish” bacteria could optimize inhibitors that fight antibiotic resistance (October 10, 2024) retrieved October 10, 2024 from
This document is subject to copyright. Except for fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.