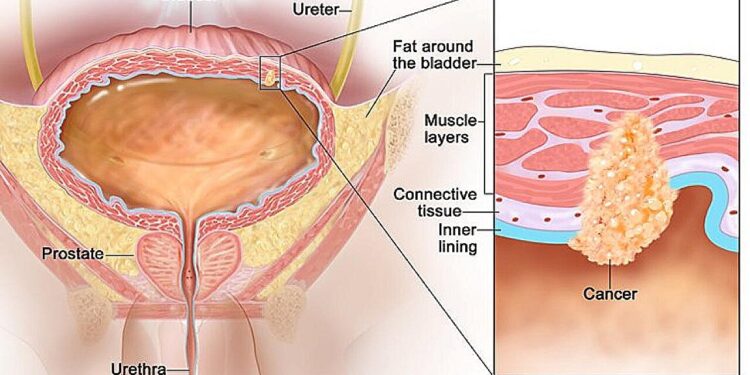
Adjuvant pembrolizumab helps people with muscle-invasive bladder cancer stay cancer-free longer than with observation alone. Credit: National Cancer Institute
Results from a large clinical trial show that immunotherapy treatment can nearly double the length of time people with high-risk, muscle-invasive bladder cancer remain cancer-free after bladder surgery. Researchers found that postoperative treatment with pembrolizumab (Keytruda), which the Food and Drug Administration (FDA) has approved for at least 18 different cancers, was superior to observation.
The study, conducted by researchers at the National Institutes of Health (NIH), is published in the New England Journal of Medicine.
“This study shows that pembrolizumab may offer patients another treatment option to help prevent their disease from coming back,” said Andrea B. Apolo, MD, principal investigator of the National Cancer Institute’s (NCI) Center for Cancer Research at the NIH. “Prolonging the time these patients are cancer-free makes a big difference in their quality of life.”
A diagnosis of muscle-invasive bladder cancer means that the bladder tumor has invaded and grown through the muscle layer that surrounds the bladder. The standard treatment for this form of bladder cancer is to surgically remove the entire bladder.
To improve the chances of success of the operation and to eliminate cancer cells that may have escaped from the tumor, patients receive chemotherapy with cisplatin during a period before the operation, called neoadjuvant therapy, or after the operation, called adjuvant therapy.
However, many people with muscle-invasive bladder cancer cannot take or refuse neoadjuvant cisplatin-based chemotherapy. Others cannot tolerate adjuvant cisplatin-based chemotherapy.
Still others, despite neoadjuvant cisplatin-based chemotherapy, have persistent muscle-invasive disease but cannot be retreated with adjuvant cisplatin-based chemotherapy. Historically, these groups of patients have been monitored more closely for signs of relapse.
As an alternative to observation, researchers have studied giving patients immunotherapy drugs after surgery to see if it can help them live longer without their cancer coming back.
In 2021, the FDA approved nivolumab (Opdivo) as an adjuvant treatment for people with high-risk, muscle-invasive bladder cancer after a clinical trial showed that the immune checkpoint inhibitor (a type of immunotherapy that releases the brakes on T cells so they can recognize and attack tumors) doubled the median time patients were cancer-free compared with a placebo. Adjuvant nivolumab is now the standard of care in this setting.
In the current trial, researchers investigated whether the immune checkpoint inhibitor pembrolizumab could also be effective as adjuvant therapy. They randomly assigned 702 patients with high-risk, muscle-invasive bladder cancer who had undergone bladder removal to receive adjuvant treatment with pembrolizumab every three weeks for one year, or to observation for the same period. About two-thirds of the patients in the trial had completed neoadjuvant treatment with cisplatin.
After a median follow-up of nearly four years, patients in the pembrolizumab group remained cancer-free for a median of 29.6 months, compared with 14.2 months for the observation group. Pembrolizumab was well tolerated, with the most common side effects being fatigue, itching, diarrhea, and an underactive thyroid.
In some types of cancer, immune checkpoint inhibitors such as pembrolizumab are more effective against PD-L1-positive tumors (meaning that the tumor cells produce a lot of PD-L1 protein on their surface) than those that are not, or PD-L1-negative. So Dr. Apolo and colleagues assessed whether the effect of pembrolizumab varied by PD-L1 status.
Among the 404 patients whose tumors were PD-L1-positive, those treated with pembrolizumab remained cancer-free for a median of 36.9 months, compared with 21 months for those in the observation group. Among the 298 patients whose tumors were PD-L1-negative, those treated with pembrolizumab remained cancer-free for a median of 17.3 months, compared with nine months for the observation group. The researchers concluded that PD-L1 status should not be used to select patients for pembrolizumab treatment because both groups benefited from adjuvant pembrolizumab.
According to preliminary overall survival data, at three years, about 61% of patients in the pembrolizumab group were still alive, compared with about 62% of patients in the observation group. The researchers noted that many patients in the observation group started taking nivolumab after it was approved or withdrew from the study, which could have confounded the results and made the overall survival data difficult to interpret.
Research teams are already building on the study results to study adjuvant therapy using various drug combinations with immune checkpoint inhibitors. Researchers are also testing biomarkers to identify patients with high-risk, muscle-invasive bladder cancer who might benefit most from any adjuvant therapy and spare those who may not need it.
More information:
Andrea B. Apolo et al., Adjuvant Pembrolizumab versus observation in muscle invasive urothelial carcinoma, New England Journal of Medicine (2024). DOI: 10.1056/NEJMoa2401726
Provided by the National Institutes of Health
Quote:Immunotherapy after surgery helps people with high-risk bladder cancer live longer without cancer, clinical trial finds (2024, September 16) retrieved September 16, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.