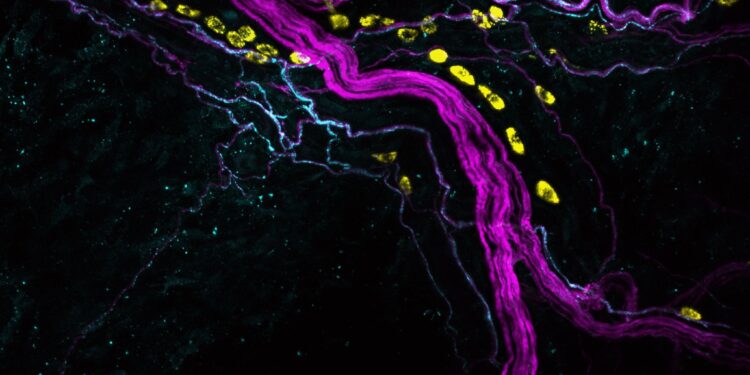
Pain neurons in the skin (magenta) and mast cells (yellow) with a subset of pain neurons (substance P+ neurons, cyan). Credit: MedUni Vienna/Rohit Jain & Shweta Tikoo
An international research group led by MedUni Vienna and IMBA – Institute of Molecular Biotechnology Vienna, has made significant progress in understanding the mechanisms that influence pain sensation after surgery.
Currently available treatment methods for postoperative pain can lead to considerable side effects and are often only partially effective. The latest findings reveal a new possibility for localized and targeted treatment. The study has just been published in Sciences Immunology.
In their research, the team led by Philipp Starkl, Shane Cronin and Josef Penninger built on previous findings regarding the role of the substance tetrahydrobiopterin (BH4) in neuropathic pain: the higher the concentration of BH4, the more intense the pain.
“It has not yet been investigated whether this correlation also applies to postoperative pain,” says Josef Penninger from the Clinical Department of Laboratory Medicine at MedUni Vienna, IMBA, University of British Columbia, Vancouver, Helmholtz Center for Infection Research, Braunschweig.
In a series of experiments in mouse models with surgically induced skin lesions and using novel analytical methods, the researchers revealed both the central role of BH4 in postoperative pain and the underlying mechanisms.
It turns out that the innate immune system plays a decisive role here. The signaling cascade triggered by tissue damage starts in special immune cells (mast cells) that are located near pain-sensing nerves in the skin and act as a production site for BH4 after surgery.
“In mice whose mast cells did not produce BH4, we observed a significantly reduced pain sensitivity after surgery. Conversely, we found that increased BH4 production by mast cells was associated with increased pain,” reports Shane Cronin from the Clinical Department of Laboratory Medicine at MedUni Vienna, IMBA.
Thanks to the key role of mast cells in pain perception, the research team has also found a possible solution to the riddle of the function of these cells in the body. “Until now, we mainly knew about their influence in allergic reactions and wondered why we had preserved this cell type over hundreds of millions of years of evolution despite its harmful and dangerous role in allergies,” says Philipp Starkl from the Department of Medicine I at MedUni Vienna.
More information:
Philipp Starkl et al., Mast cell-derived BH4 and serotonin are key mediators of postoperative pain, Sciences Immunology (2024). DOI: 10.1126/sciimmunol.adh0545
Provided by the Medical University of Vienna
Quote:Postoperative pain mechanisms reveal an avenue for localized and targeted therapy (2024, August 26) retrieved August 26, 2024 from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.