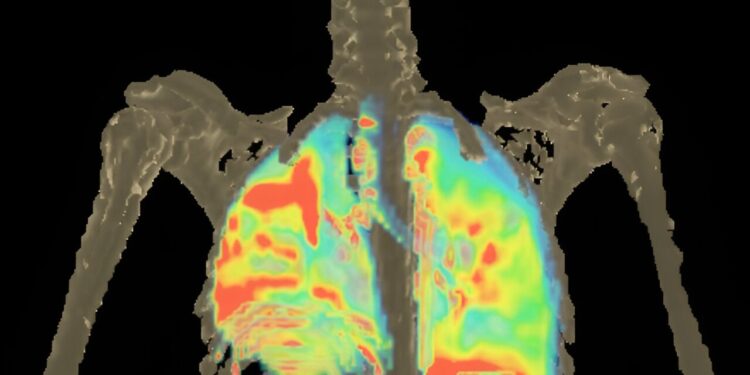
Exposure to 18F-pretomanid in brain and lung tissues of a patient with active tuberculosis. Credit: Sanjay Jain Lab
In a preliminary study involving small numbers of humans, rabbits and mice, researchers at Johns Hopkins Children’s Center say they have developed four new treatment regimens that could treat and save the lives of people with multidrug-resistant (MDR) tuberculosis meningitis.
Although tuberculous meningitis, which affects the brain and spine, is extremely rare in the United States, it is believed to be the most deadly form of tuberculosis worldwide.
In a report published on August 14 in Nature CommunicationsThe researchers present the treatment regimens, mainly composed of antibiotics already approved by the American Food and Drug Administration (FDA) for other uses, or of antibiotics currently in clinical trials.
The study researchers say these regimens could be easily evaluated in new clinical studies or used now to treat people with multidrug-resistant TB meningitis on a case-by-case basis.
According to the World Health Organization, tuberculosis remains a global public health threat, with the highest number of cases occurring in the South-East Asia region and Africa, and is one of the leading killer diseases caused by a single infectious agent, the tuberculosis bacillus.
There is no FDA-approved antibiotic treatment specifically effective against tuberculous meningitis, although antibiotic treatments developed for pulmonary tuberculosis are widely available.
A previous study from Johns Hopkins Children’s Center led by Dr. Sanjay Jain, senior author of the new study and director of the Johns Hopkins Center for Infection and Inflammation Imaging Research, showed that the FDA-approved regimen of three antibiotics currently used to treat drug-resistant pulmonary tuberculosis — bedaquiline, pretomanid, and linezolid (BPaL) — is not effective in treating tuberculous meningitis because bedaquiline and linezolid cannot effectively cross the blood-brain barrier — a network of cells that prevents germs and toxins from entering the brain.
The new study used positron emission tomography (PET) and computed tomography (CT) technology on people, rabbits and mice to show how different antibiotics enter the brain and other areas of the body, says Jain, who is also a pediatric infectious disease specialist at Johns Hopkins Children’s Center.
For the new experiments, the researchers first created a chemically identical, scan-friendly version of the antibiotic pretomanid, and conducted a whole-body study on eight people: six healthy volunteers and two patients newly diagnosed with pulmonary tuberculosis.
Using PET and CT imaging, the researchers measured the antibiotic’s penetration into brain and lung tissue and found that pretomanid penetrated the brain more than twice as well as the lungs of all human subjects. Pretomanid levels in cerebrospinal fluid (CSF) were also different from those in the brain.
“We found that antibiotic levels in CSF often have no relationship to those in the brain,” said Dr. Xueyi Chen, one of the study’s first authors and a pediatric infectious diseases researcher at Johns Hopkins University School of Medicine.
Then, using PET imaging, the researchers tested four different antibiotics (chemically identical, imageable versions) active against multidrug-resistant TB (pretomanid, sutezolid, linezolid, and bedaquiline) and their penetration into lung and brain tissues in mouse and rabbit models of tuberculous meningitis.
All four antibiotics were well distributed throughout the body, but their penetration into brain and lung tissues was significantly different. While pretomanid levels were significantly higher in brain than in lung tissue, sutezolid, linezolid, and bedaquiline had levels at least three times higher in lung tissue, with bedaquiline having levels almost ten times higher than in brain.
“Interestingly, brain concentrations of pretomanid were two times higher than those in plasma. In contrast, while brain concentrations of bedaquiline were almost five times higher than those in plasma, lung concentrations were two times higher than those in plasma. This preferential accumulation of different antibiotics in brain or lung tissue is very important and explains why some antibiotics are very effective in the lungs but not in the brain and vice versa,” says Jain.
The researchers then created computer models that parallel and measure the behavior of the drugs in living systems, called pharmacokinetics, for pretomanid, sutezolid, linezolid, and bedaquiline. Mathematical simulations based on the models were then used to predict what tissue exposures and doses would be needed to achieve therapeutic brain penetration of each antibiotic.
Only pretomanid achieved therapeutic brain tissue exposures at the standard human oral dose. Even at a dose four times the standard human oral dose, brain tissue exposures to bedaquiline are expected to be only one-third of target levels.
The researchers found that all three pretomanid-based multidrug regimens (BPa50LZ (bedaquiline, pretomanid, linezolid, pyrazinamide), Pa100LZ (pretomanid, linezolid, pyrazinamide), and Pa50LMxZ (pretomanid, linezolid, moxifloxacin, pyrazinamide)) were highly effective in treating tuberculous meningitis in animal models when given at a dose equivalent to that in humans.
The ability of each regimen to kill bacteria in the brain was several times greater than that of the standard TB treatment (R10HZ) and the BPaL regimen (BPa50L).
Because multidrug-resistant TB strains can also be resistant to pyrazinamide, the researchers developed a fourth, non-pyrazinamide regimen: Pa100SMx (pretomanid, sutezolid, moxifloxacin). They found that it was as effective as standard first-line TB treatment and reduced bacterial load in the brain ten times more effectively than the BPaL regimen.
The researchers cautioned that their experiments were limited by the small amounts of the imageable version of the antibiotics used per subject. However, several studies support the idea that administering small amounts of a drug is a reliable indicator of a drug’s bodily distribution.
More information:
Nature Communications (2024). www.nature.com/articles/41467-024-50989-4
Provided by Johns Hopkins University
Quote:Researchers report potential new treatment regimens for multidrug-resistant tuberculosis meningitis (2024, August 14) retrieved August 14, 2024, from
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.