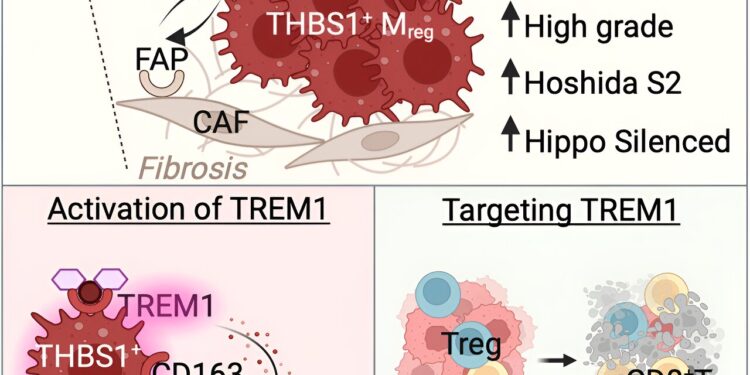
Graphical summary. Credit: Cell Reports (2024). DOI: 10.1016/j.celrep.2024.11377
A research team composed of Canadian and French scientists, led by Professor Maya Saleh of INRS, is studying resistance to immunotherapy in certain patients with hepatocellular carcinoma (HCC) associated with steatotic liver disease. The results are published in the journal Cell Reports.
Hepatocellular carcinoma is associated with known risk factors such as chronic hepatitis B or C infection, alcohol abuse, and metabolic dysfunction. It is the most common type of liver cancer. Despite major advances in immunotherapy, this cancer is often fatal: approximately 75% of patients with advanced HCC do not respond to this type of treatment for reasons that remain to be elucidated.
This encouraged the research team to explore the link between liver disease associated with metabolic dysfunction, chronic inflammatory liver disease, and therapeutic resistance to immunotherapy in HCC patients.
“We have identified an immune biomarker for HCC associated with steatotic liver disease, which will allow us to develop new immunotherapies,” explains Professor Maya Saleh, international specialist in immuno-oncology. “We could consider immunotherapies that restore an effective immune response against HCC by attenuating damaging inflammation in the liver.”
Discovery of a potential therapeutic target
HCC remains a major public health problem; in North America, its incidence has doubled over the past three decades. Before the approval of immunotherapy, treatment options for advanced HCC were limited and ineffective. For example, sorafenib improves average overall survival by only 3 months and is associated with significant side effects.
Immunotherapies, when administered in combination, increase the average survival of patients with HCC by an average of 17 months.
Thanks to the use of “omics” technologies, which make it possible to analyze large quantities of biological data in a short time, the team developed an immune map of the tumor and the adjacent non-tumor liver in 10 patients. These first immune maps led them to study databases of hundreds of patients in order to validate the immune profiles linked to risk factors and associated with the severity of the disease.
These initial results indicate that chronic inflammation due to fatty liver disease makes the liver cancer environment unique, with an expansion of immunosuppressive cells that paralyze the tumor’s immunological attack.
The research team demonstrated that immunosuppressive cells express an inflammatory receptor called TREM1, which makes them more dangerous. They therefore highlighted TREM1 as a potential therapeutic target in HCC associated with steatotic liver disease.
Interesting implications for immunotherapy research
By identifying this biomarker, which could explain treatment failure in people with HCC, the team has paved the way for a new approach to patient classification. This would allow them to determine who would be most likely to respond to immunotherapy before treatment even begins.
Such a scientific advance would alleviate the psychological burden of patients who do not respond to immunotherapy. Significant physical impacts, including side effects, could also be avoided.
“This is a promising avenue for the coming years. We will continue the analysis by characterizing the immune component of tumors in a larger cohort of patients, including comprehensive imaging of tumor cell composition and the use “artificial intelligence to link immune profiles to response to therapy. This could have a significant impact in the field,” concludes Professor Saleh.
More information:
Julie Giraud et al, THBS1+ myeloid cells develop in SLD hepatocellular carcinoma and contribute to immunosuppression and poor prognosis via TREM1, Cell Reports (2024). DOI: 10.1016/j.celrep.2024.11377 www.cell.com/cell-reports/full … 2211-1247(24)00101-3
Quote: Liver cancer: a promising avenue for more effective immunotherapies (February 14, 2024) retrieved on February 14, 2024 from
This document is subject to copyright. Apart from fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.